Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Kelash Kumar1*, Harold Matos-Casano2, Yash Patel3, FNU Poonam4, Karthik Seetharam5
1Department of Internal Medicine, Maimonides Medical Center, BROOKLYN, USA
2Department of Internal Medicine, Wyckoff Heights Medical Center, BROOKLYN, USA
3Department of Internal Medicine, Wyckoff Heights Medical Center, Brooklyn, USA
4Department of Internal Medicine, Wyckoff Heights Medical Center, BROOKLYN, USA
5Department of Internal Medicine, Wyckoff Heights Medical Center, BROOKLYN, USA
*Corresponding Author: Kelash Kumar, Department of Internal Medicine, Maimonides Medical Center, BROOKLYN, USA.
Received: May 25, 2022
Accepted: May 31, 2022
Published: June 03, 2022
Citation: Kelash Kumar, Harold Matos-Casano, Yash Patel, FNU Poonam, Karthik Seetharam (2022) “Seasonal Influenza-A virus infection Resulting in Acute Myopathy and Myocarditis Followed by Heart Failure”, Aditum Journal of Clinical and Biomedical Research, 3(7); DOI: http;//doi.org/07.2022/1.137.
Copyright: © 2022 Kelash Kumar. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Respiratory tract infections due to influenza virus are commonly observed. Occasionally, influenza infections may present or be associated with extra-pulmonary complications. In particular, the concurrence of influenza myocarditis and myopathy is rarely observed. We present the case of an elderly woman without prior cardiac disease showing distinct but overlapping presentations of influenza myocarditis and myopathy, who progressed to develop clinical signs of heart failure following the resolution of the respiratory illness. The case serves to alert clinicians to consider the presence of subclinical presentations of influenza myocarditis in elderly patients and to monitor the development of signs of heart failure after the resolution of symptoms.
Introduction
Influenza is commonly restricted to the respiratory system. Extra-pulmonary manifestations are less common and can complicate a typical presentation [1]. Myocarditis and myositis are extra-pulmonary conditions which occur infrequently but can lead to life-threatening complications [2]. We describe the case of an elderly female who became disabled due to myositis after a few days of typical flu-like symptoms which later led to development of congestive heart failure (CHF) upon resolution of her respiratory symptoms.
Case Presentation
A 77 year-old female with a history of osteoarthritis was brought to the hospital after she was found immobile at her residence. The patient complained of headaches, malaise, anorexia, fever, chills, nasal discharge and cough productive of clear sputum over two days prior to her arrival. She reported a profound weakness that made her unable to stand up. Furthermore, she used her elbows to drag herself around her house during the rest of the morning, until becoming severely fatigued and unable to move at all. Later she was found lying on the floor. She denied having any allergies, past surgeries, and drugs. Vaccine history was unknown.
Her physical exam was notable for a temperature of 100.6 ℉, blood pressure 110/67 mmHg (mean arterial blood pressure 81 mmHg ), heart rate of 100 beats per minute and respiratory rate 20/min. Pulmonary auscultation revealed bilateral rhonchi. Proximal lower extremity weakness of 3/5 was noted. Muscle tenderness was absent. Remaining physical exam was unremarkable.
Significant laboratory findings included a white blood cell count of 11,000 K/UL, creatine kinase of 7904 U/L (relative index 0.4), aldolase 43.5 U/L, myoglobin 19.7 nmol/L, troponin I of 9.74 ng/mL, C-reactive protein was 132 mg/L and thyroid stimulating level (TSH) 1.32 mIU/L ( Table 1 ). Rapid viral antigen detection test was positive for influenza A. Electrocardiogram did not show findings consistent with ischemic changes, arrhythmia or ventricular hypertrophy.
|
Test |
Result |
Reference range |
|
White blood cell count |
11,000 K/UL |
4.8 – 11.8 K/UL |
|
Creatinine Phosphokinase |
7904 IU/L |
24 – 205 IU/L |
|
Aldolase |
43.5 U/L |
1.0 – 7.5 U/L |
|
Myloglobin |
19.7 nmol/L |
1.28 – 3.68 nmol/L |
|
Troponin |
9.74 ng/ml |
0.00 – 0.02 ng/d |
|
C-reactive Protein |
132 mg/ dl |
0.00 – 0.90 mg/dl |
|
Thyroid stimulating hormone |
1.32 mIU/L |
0.5 – 5.0 mIU/L |
Table 1: Laboratory values
Supportive treatment was initiated with IV crystalloids, analgesics and Oseltamivir even though patient had been symptomatic for more than 48 hours.
Echocardiogram on day 2, revealed an ejection fraction of 55-60%. On the same day, the patient developed acute-onset shortness of breath and tachycardia. Computed tomography of the chest with contrast showed bilateral lower lung infiltrates with predominance on the right (Figure 1) and upper lobe ground-glass opacities.

Figure 1: Computed tomography of the chest with contrast showing bilateral lower lung infiltrates predominantly on the right side as shown by red arrows.
Shortly afterwards, her symptoms further aggravated and she became hemodynamically unstable as her systolic blood pressure and consequently mean arterial pressure dropped to 57 mmHg. IV fluids were uptitrated and antibiotics Vancomycin with Azithromycin were initiated. Urine streptococcal antigen was positive and Klebsiella pneumoniae was subsequently isolated on urine culture. The antibiotic regimen was changed to intravenous Levofloxacin after 4 days and her symptoms gradually resolved.
The patient's ability to stand and gait endurance gradually improved over several days. On day 9, the patient began complaining of shortness of breath, with pressure-like chest discomfort. Rales were auscultated. A portable chest X-ray showed a slightly enlarged cardiac silhouette and prominent vascular markings with flow cephalization (Figure 2). Brain Natriuretic Peptide was 244.7 pg/mL. No consolidations were visualized. These findings were suggestive of congestive heart failure and 40 mg of furosemide were administered intravenously with symptom improvement reported a few hours later. The patient was discharged home on day 12 on per oral Furosemide 20 mg per day as needed. On 3 week followup in outpatient clinic, patient had developed +2 bilateral pitting edema of the lower extremities.
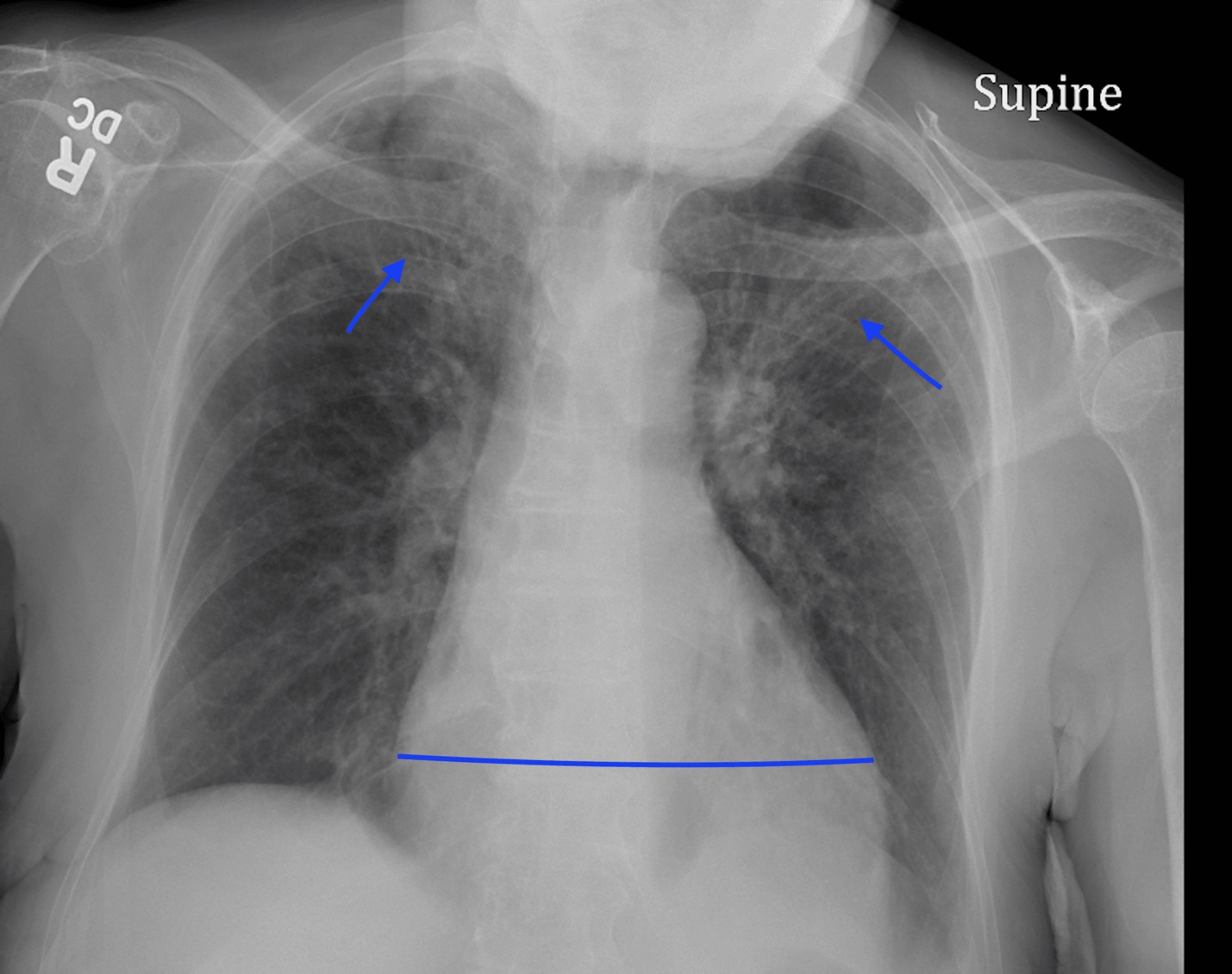
Figure 2: X-ray chest showing bilateral cephalization of pulmonary vascular flow and enlarged cardiac silhouette
Discussion
Influenza is generally associated with respiratory involvement, the prevalence and burden of its extrapulmonary manifestations are unknown [3]. Myocarditis and myositis have been reported as complications of influenza. Most reports have described occurring separately. Rarely do they occur simultaneously.
Myocarditis has been clinically diagnosed in an estimated 0.4 to 13% of adults hospitalized with influenza [4]. It may occur in the absence of more severe respiratory complications. The most common viral subtype being A (H1N1) pdm09. The clinical course is variable, with symptoms of cardiac dysfunction appearing around days 4 to 7 after initial presentation [5]. Most cases are asymptomatic. Congestive heart failure is the most common complication; many require advanced cardiac support therapies [6]. 70% of patients with congestive heart failure experience full recovery within 20 days after the onset of dysfunction [7]. Diagnosis is with cardiac enzymes, echocardiogram and endomyocardial biopsy. Cardiac Magnetic Resonance Imaging is considered a modality of choice to evaluate the extent of disease and possible biopsy sites.
Myositis is thought to be relatively more common when compared to myocarditis. It often affects women under 60, who are afflicted by influenza A. It may be more common in the elderly than actually recognized [8-9]. Its diagnosis is established clinically and supported by markers such as CK-MB, aldolase and myoglobin. Treatment is primarily symptomatic in both conditions.
The occurrence of both extra-pulmonary complications during a single episode of influenza has been rarely reported. Most reported cases have been in young females. Our case is unique in two regards. First, the presentation of both complications in an elderly female. Second, the biochemical abnormalities characteristic of each were present during this admission but occurred at different times. The patient did not report any myalgia or calf tenderness, but the myositis still resulted in significant functional impairment. Considering the atypical features, the patient’s symptoms may have been attributed to dehydration and deconditioning. The use of Troponin I and CK-MB facilitated the diagnosis and identification of the both causes and congestive heart failure.
Furthermore, it is thought that the use of Oseltamivir in this patient may have contributed to decrease the severity of both complications [10].
Acute coronary syndrome (ACS) was considered on admission. However, Pt did not complain of chest pain and shortness of breath. No cardiac risk factors like hypertension, hyperlipidemia, diabetes mellitus, or cigarette smoking history. No ischemic changes on electrocardiogram and no wall motion abnormalities on echocardiogram points against ACS. Furthermore, in the setting upper respiratory tract symptoms, muscle weakness, elevated inflammatory markers and down trending troponin with anti-viral and symptomatic management like IV fluids points against ACS. Given above findings and the patient clinical condition, coronary angiogram was deferred until outpatient evaluation.
We do not have the definitive diagnosis of Myocarditis (endomyocardial biopsy) but the patient did meet the criteria of 2013 European Society of Cardiology (ESC) position statement on clinically suspected myocarditis [11]. Clinical presentation of New-onset (days to three months) or worsening of dyspnea at rest and/or exercise, fatigue with or without left and/or right HF signs and diagnostic criteria of elevated troponin.
The continued presence of heart failure symptoms at her follow-up clinic visits suggests congestive heart failure. This is notable, in view of the findings of a recent study which found an increase in heart failure hospitalizations during periods of increased influenza activity [12]. Since the patient only experienced these symptoms after she had myocarditis, we believe that this is the underlying etiology of her heart failure.
Conclusions
We present a patient with profound myositis and acute respiratory illness which were followed by heart failure in an elderly female. Most cases have been reported in younger females. In view of the atypical presentations, we suggest the providers should have low threshold to monitor the development and progression of the extra-pulmonary complications of Influenza specifically myositis, myocarditis and overt heart failure, especially in elderly patients. Lack of prior vaccination against Influenza could lead to development of extra-pulmonary complications . We also suggest Oseltamivir within 5 days of respiratory symptoms to decrease the severity of complications.