Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Takeyoshi Shimoji1*, Takaoki Kimura2
1Neurosurgery, Okinawa Central Hospital 1-26-6 Yogi Naha Japan
2Division of Pediatric neurosurgery, Shin-Yurigaoka general hospital
*Corresponding author: Takeyoshi Shimoji, Neurosurgery, Okinawa Central Hospital 1-26-6 Yogi Naha Japan.
Received Date: January 16, 2022
Accepted Date: January 20, 2022
Published Date: January 25, 2022
Citation: Takeyoshi Shimoji, Takaoki Kimura (2022) “Treating Craniosynostosis Based on Skull Base Pathology.” Clinical Case Reports and Clinical Study, 7(2); DOI: http;//doi.org/01.2022/1.126.
Copyright: © 2022 Takeyoshi Shimoji. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Psychologists have reported that, despite surgery done during infancy, a certain percentage of intellectual and behavioral problems appeared at the time of such patients’ admission to elementary school. We report the long-term outcomes of our approach, focusing on the removal of the heavily overgrown sphenoid ridge. This report may address their concerns.
Methods: Seventeen children were included in total, with diagnoses of scaphocephaly (n = 5), brachycephaly (n = 4), plagiocephaly (n = 2), and trigonocephaly (n = 6). All cases were non-syndromic typical synostosis. All patients underwent three-dimensional computed tomography (3D-CT) for definitive diagnosis. These four pathologies, exhibited small, underdeveloped anterior cranial fossae and medially displaced pterion regions compared to normal anatomy. In addition, abnormally wide sphenoid ridges were noted during operation. These pathologies constricted the frontal cranium, and it was anticipated that they would make it smaller than normal and compress the pars opecularis (mirror neurons). Based on the findings of the imaging study, front-orbital advancement (FOA) was planned to extend the remodeling to the anterior cranial fossae. Since it was confirmed that the sphenoid ridges protruded widely posteriorly and were strangling the mirror neurons, they were removed to the meningo-orbital band.
Results: After the treatment, most of cases diagnosed in infancy grew up keeping these conditions for a long time. The cases diagnosed after one year old tend to have delayed development. They also made some improvement after treatment.
Conclusion: It is important to enlarge the anterior cranial fossae using FOA in each case and remodel the greater/lesser wings and sphenoid ridges. This method keeps children in developing well during long-term follow-ups.
Introduction
Reports on treatments of craniosynostosis (CS) include the conventional method of simply removing affected sutures to the adding of FOA [11] by Hoffman et al., using distractions [10], and, more recently, incorporating a helmet after removing the suture using an endoscope [12,24].
In general, the goal of treatment of CS is to improve cosmetic problems and prevent brain dysfunction that may occur in the future [31]. In the 1990s, psychologists at European and North American centers reported that, despite surgery done during infancy, a certain percentage of intellectual and behavioral problems appeared at the time of admission to elementary school [3,14,34]. These reports are considered to pose a very major problem to those performing treatment.
In this paper, we summarize and report the results of the typical non-syndromic craniosynostosis surgery cases we performed, which were followed up for 2.7 to 16 years (average 9.2 years), taking into account the opinions of psychologists.
Subjects and methods: Seventeen patients, who were first seen with a chief complaint about their cranial shape, were treated at Okinawa Pref. Nanbu Medical Center & Children’s Medical Center (16cases) and Sin-Yurigaoka general hospital (1 case) between 2006 and 2018. The definitive diagnosis was made by 3D-CT. All patients underwent magnetic resonance imaging to confirm the absence of morphological abnormalities in the brain.
All patients were judged to have surgical indications for typical non-syndromic CS, and cranioplasty was performed as early as possible.
Cases
Scaphocephaly (Table 1; cases 1–5): five cases. For the first three cases, a craniectomy was performed and an expanded suturectomy. Morphologically, the first patient had a somewhat navicular shape after surgery, which was not a satisfactory result. Urinary incontinence was observed at the age of 6 years, and there seemed to be some intellectual problems, but the child scored 96 on an IQ test and progressed to ordinary elementary and middle school, later advancing to an agriculture and forestry high schools (Fig. 1a) (case 1). In the second case, there was no problem with development, especially cosmetically (Fig. 1b) (case 2). The third case was diagnosed at 6 months of age, and a craniectomy that was expanded more than usual was performed. There was no speech at 1.5 years, and when a 3D-CT scan was taken, a slight triangular shape was observed and decompressive cranioplasty was enforced. Since the operation, there has been a catch up in development and it has become possible for the child to live normally. However, some intellectual problems persist, and the child is enrolled in a support class (Fig. 1c) (case 3).
|
Diagnosis |
Case No. |
Sex |
Age at surgery |
Follow-up period |
Signs and symptoms |
Status after surgery |
Present status |
|
Scaphocephaly |
1 |
M |
11m |
16y |
Good development |
IQ: 96 |
Attends an Agriculture and Forestry High School |
|
2 |
M |
6m |
16y |
Good development |
No development problems |
Attends a regular high school |
|
|
3 |
M |
6m |
11.3y |
Good development |
Scaphocephaly treated at 3 m/o |
Attends junior high school in the support class |
|
|
4 |
F |
1.5y |
9.7y |
Good development |
Started talking well immediately after the operation. |
Attends elementary school, get good grades |
|
|
5 |
M |
6m |
6.2y |
Good development |
Maintains good development |
Attends elementary school |
|
|
Brachycephaly |
6 |
F |
8m |
9.2y |
Good development |
Maintains good development |
Attends elementary school |
|
7 |
F |
5m |
15y |
Good development |
Maintains good development |
Attends normal junior high school |
|
|
8 |
F |
3y9m |
13.4y |
Good development |
Maintains good development |
Attends normal high school, second grade |
|
|
9 |
F |
2y |
3.3y |
No words yet, noticeable motor delay |
Able to sit after operation for 3m |
Incomprehensible words |
|
|
Plagiocephaly |
10 |
M |
1y |
14.5y |
Cannot sit without support |
Improved motor activities |
Attends normal junior high school |
|
11 |
F |
7m |
6.4y |
Good development |
Steady development |
Attends elementary school |
|
|
Trigonocephaly |
12 |
F |
1y |
8.1y |
Sitting with three points |
Post-op, 4m: acquired a couple of words and steadily sitting |
Attends elementary school, third grade |
|
13 |
M |
1.5y |
7.8y |
Speaking a few words only |
Post-op, 3m: running, ceased head banging, and acquired 10 words |
Attends third-grade support class |
|
|
14 |
M |
3y4m |
7y |
Difficulty to control head movements |
Not speaking, sitting with three points, |
Speaks no understandable words |
|
|
15 |
M |
5y6m |
6.4y |
Only started to walk at 3y/o |
Post-op, 4 years: able to say two sentenses |
Able to stand with support |
|
|
16 |
F |
4y6m |
4y |
No speech development |
Post-op, 1.5 years: understands what her mother says |
Attend special school |
|
|
17 |
M |
11m |
2.7y |
No control over head movements |
Post op, day 11: Able to control head movements |
Mastered a few words |
Table 1: Summary of the patients M; male F; female
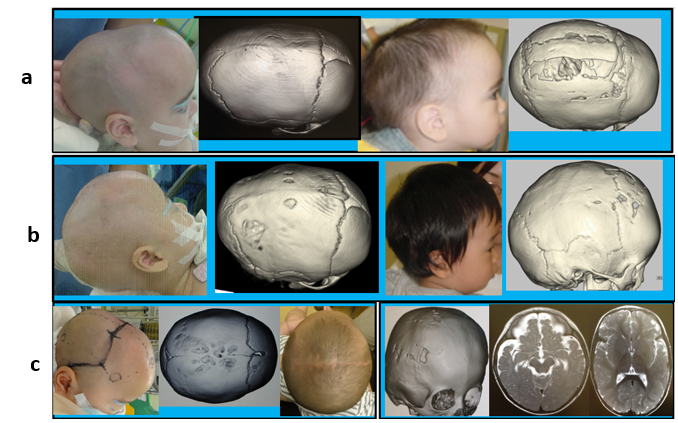
Fig. 1: Scaphocephaly 1
a: In the first case, suturectomy resulted in a relatively long head (Table 1;1)
b: In the second case, suturectomy resulted in a good outcome (Table 1;2)
c: In the third case, suturectomy resulted in a good outcome (left column). One year later the patient developed mild trigonocephaly, which was successfully treated (right column) (Table 1;3)
In the remaining two cases (Table 1; cases 4–5), a depression of pterion was remarkable and slight frontal bossing was recognized. A 3D-CT scan also showed frontal narrowing. After the performance of the expanded craniectomy, a frontal craniotomy was carried out, and it was observed that the sphenoid ridge was thin and wide, so it was removed. It was then judged necessary to expand the anterior skull base, and FOA was carried out (Fig. 2). Both cases developed normally postoperatively.

Fig. 2. Scaphocephaly 2
a: The first two pictures show the closed sagittal suture and smaller anterior fossae. Expanding parietal suturectomy and bifrontal craniotomy were performed, and the supraorbital bar was created. Abnormal overgrowth of the sphenoid ridges (surgical findings) were removed (black arrows) and expanded the anterior fossae.
b: Preoperative and postoperative images of the fourth case (Table 1; 4)
c: Preoperative and postoperative images of the fifth case (Table 1; 5)
Brachycephaly (Table 1; cases 6–9): four cases. Two cases were operated during infancy and one case at 3 years old (Fig. 3) (Table 1; cases 6–8). These cases all showed good long-term progress without any developmental problems. In another case, the patient (Table 1; case 9), who was seen at the age of 2 years, did not speak any significant words, was unable to sit, and had marked salivation. After the operation, the sitting position became possible after 3 months, and the child became able to express emotions. The salivation drastically decreased. At present, she speaks no significant words and is in a kneeling position.
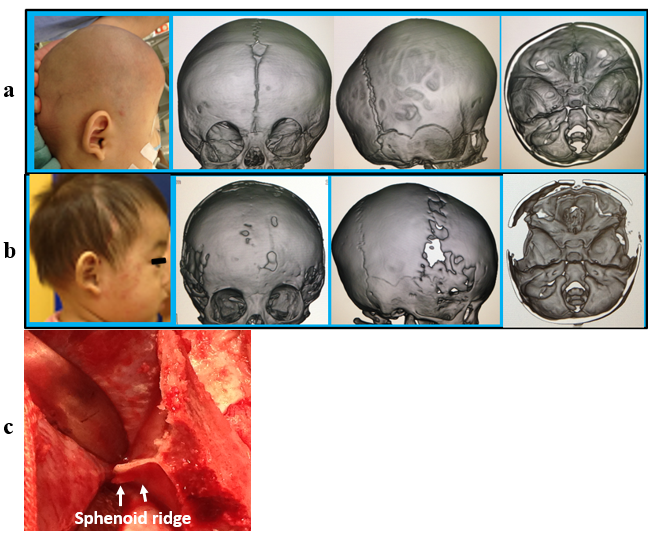
Fig. 3. Brachycephaly (Table 1; 6)
a: Preoperatively, the child’s skull was brachycephalic (short in length). A 3D-CT scan showed closed bilateral coronal sutures and small anterior cranial fossa.
b: Postoperatively, brachycephaly improved, and a 3D-CT scan showed improved brachycephaly and an enlarged anterior cranial fossa.
c: The sphenoid ridge (surgical findings).
Plagiocephaly (Table 1; cases 10–11): two cases (Fig. 4). One patient(case10) had a medical examination at 9 months due to symptoms such as not being able to sit by himself and not being good at crawling. He was diagnosed by 3D-CT scan, and cranioplasty was carried out at age 1. Improvement of the symptoms was observed immediately after the operation, and the child grew without any developmental problems after that, entering ordinary elementary school. He is currently enrolled in a high-level middle school (Fig. 4, case 10). The second patient was seen at 4 months for an abnormal craniofacial shape. There was no problem in her development. An operation was carried out at 7 months, and distortion of the face also improved gradually afterward. Currently, she is in a regular first grade in elementary school (Fig. 4 case 11).

Fig. 4. Plagiocephaly
a: First case pre-op. (Table 1; 10): Child’s face was distorted. A 3D-CT scan showed left coronal synostosis and small anterior cranial fossae.
Post-op. (right two images): Surgery enlarged the anterior cranial fossa and reduced the facial distortion.
b: Second case (Table 1; 11), ZS: Child’s face was distorted. A 3D-CT scan showed right coronal synostosis and small anterior cranial fossae.
Post-op. (right two images): Surgery reduced the facial distortion and enlarged the anterior cranial fossae.
c: Abnormal overgrowth of the sphenoid ridge.
Trigonocephaly (early fusion of the frontal suture; Table 1; cases 12–17): six cases. One patient who underwent surgery immediately after her first birthday grew satisfactorily and is now in ordinary second grade of elementary school (case 12). There was only one operation in infancy (Fig. 5, case 17), and at presentation, there was no neck stability and a considerable delay in development. Neck stability became possible 11 days after operation. One month after the operation, the child began to look at other people’s faces, laugh well and be able to sit for one minute. However, at 3 years and 7 months old, he made little improvement like he is difficult to sit for long time and move by himself and only speaks a few words.
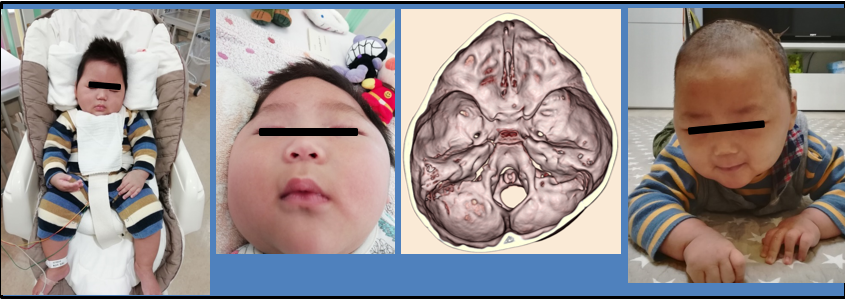
Fig. 5. Typical trigonocephaly (Table 1, 1, IA)
First image showing 11m/o boy with no neck control. The forehead showed triangular deformity. A 3D-CT scan showed a triangular forehead and small anterior fossae.
The fourth image shows the patient 11 days post-operatively, neck control was observed, and the forehead became flatter and bigger.
One case had a medical examination at one and a half years and only spoke the two words papa and mama, could only barely sit up, exhibited self-injurious action such as hitting his head on things, and had a terrible temper. Cranioplasty was performed at the age of one and a half years. He was able to run 3 months after the operation, and the self-injurious actions disappeared. The number of words gradually increased, and it was reported that there was no delay in nursery school compared to other children. However, some intellectual issues remained, and at present, he is enrolled in a support class in third grade in elementary school (case 13). The other three patients were seen at the ages of 3 to 5 years and had severe intellectual disabilities. After surgery, some improvements in terms of language, comprehension, and exercise were seen (cases 14–16).
Surgical Procedures
For the scaphocephaly, expanded suturectomy of the parietal region was carried out in the first three cases. In the fourth and fifth cases, a narrow forehead and the anterior cranial fossae were present, and an overgrowth sphenoid ridge was found during operation. The sphenoidal ridge overgrowth was confirmed for the other three pathologies as well. Thus, the frontal region was subjected to the following surgical techniques.
A coronal incision of the scalp, including the periosteum, was made to expose the bilateral supraorbital ridges well, and a bilateral frontal craniotomy was performed.
Next, an orbital bar was made using a high-speed drill incised just above front-zygomatic suture of the lateral orbital walls on both sides, rounded up to the base of the frontal skull by a several millimeters wide, the ceiling of the orbit was incised in a V-shape, an osteotomy was performed linearly at the inferior border of the frontal bone in the central part, after which the innermost part of the orbit was cut, and the supraorbital bar was removed as a lump. In the supraorbital bar of the trigonocephaly, the raised part of the nasion was cut, and a splint was applied to straighten it (Fig. 6d). Second, both sides of the sphenoid bone were largely removed, and both sides of the sphenoid ridges were removed until the orbito-meningeal band. During closure, a supraorbital bar placed a small bone fragment on the lateral side of the orbit and moved them forward. A small hole was placed outside the orbit and loosely fixed with an absorbing thread. A substantial part of the frontal bone was removed and returned with a floating method. The scalp was closed by a burying method (Fig. 6).

Fig. 6. Operation
a: The scalp, including the pericranium, was reflected down to the bilateral superior orbit and secured.
b: After bifrontal craniotomy, the orbital bar was taken out and the greater sphenoid wing was removed with a rongeur.
c: The overgrowth of the sphenoid ridge was bilaterally removed.
d: In cases of trigonocephaly, the orbital bar was cut at the midline and fastened to a brace using the stripped frontal bone to make it linear in shape.
e: The orbital bar was replaced in the skull. Small bone strips were placed laterally and posteriorly to be advanced anteriorly.
f: A considerable amount of the bone was removed at the closure step.
Discussion
The purpose of the treatment of CS is to improve cosmetic problems and to prevent the brain dysfunction that may occur in the future [31].
The typical CS cases are generally treated in infancy [2,16, 21, 23].
In our cases, presentation in infancy was only in four out of five cases of scaphocephaly, two of four cases of brachycephaly, one of two cases of plagiocephaly, and one of six cases of trigonocephaly. These typical cases should be diagnosed and treated in infancy, but delayed presentation is seen in many cases. The same trend has been observed at other institutions in Japan [21]. Renier et al. [27] reported that many cases diagnosed after the age of 1 year may result in increased intracranial pressure and affect mental function. In our cases, the rate of complication for developmental delay was high in the cases where delayed treatment was conducted.
Total remodeling, such as Renier’s H technique [8, 20] and the Pi method by Jane et al. [4], were adopted because the operation method for scaphocephaly cannot obtain good results only through suturectomy. Rottgers et al. [29] perform two-thirds of remodeling in the front of the skull, address the narrowing of the frontal area with a fracture of the temporal bone, and perform FOA if hypotelorism or supraorbital rim retreat occurs. In our five cases of scaphocephaly, three cases were undergoing expanded suturectomy and were improved from the preoperative level in terms of cosmetic view. However, the first case was suspected of having incontinence and mild intellectual impairment at the age of 6 years, and the second case was pointed out to have intellectual delay at the age of one and a half years, and a re-examination revealed fusion of the frontal suture. Therefore, we thought that there were some cases in which the therapeutic effect of conventional therapy was inadequate. In two cases subsequently diagnosed, the depression of the pterional region and the narrowing of the frontal region were recognized, and in addition to expanded suturectomy of the parietal region, a bilateral frontal craniotomy and FOA were carried out, and, in addition, the sphenoid greater and lesser wings, along with the overgrowth sphenoid ridge discovered during the operation, were deliberately removed.
Plagiocephaly is a union of unilateral coronary sutures. Facial distortion is a serious problem. Computed tomography depicts the distortion of the entire skull (Fig. 4). Di Rocco et al. [7] classify such cases according to the degree of skull base distortion. Both of our cases correspond to the IIB of the classification. Since the report on FOA for plagiocephaly by Hoffman et al. [11] in 1976, there have been many reports on the treatment of plagiocephaly by incorporating this technique [13,16,18,22]. Mesa et al. [18] created a supraorbital bar after bilateral frontal craniotomy, which was formed by coronal and sagittal plane. Our method is similar to this, but we also remove the sphenoid greater and lesser wings along with the sphenoid ridge. As a result, the distortion of the face is also improved. FOA is also indicated for the treatment of brachycephaly [1, 16, 17, 36] and trigonocephaly [17, 19]. For trigonocephaly, Marchac [15] straightens the orbital bar with a green-stick fracture, but we remove the hyper ossified and bulging part of the orbital bar in trigonocephaly and place a splint on it. In these pathologies in our cases, we also observed overgrowth sphenoid ridge. In previously reported cases of CS, descriptions of abnormal sphenoid ridges cannot be found except for in our reported cases of mild trigonocephaly [32, 33]. In 1971, Seeger and Gabrielsen [30] confirmed the finding that the front-sphenoidal suture was closed and the anterior fossa was shortened based on an X-ray and commented that resection of the coronal suture alone would not be enough for the operation. Plooij et al. [25] also reported a case in which the front-sphenoidal suture closed, which caused plagiocephaly, even after the work by Francel et al. [9] in 1995. There is an additional report of sphenoid ridge duplication in Tokumaru et al. [35]. In 1977, Raimondi and Gutierrez [26] described attempting to expand the frontal and temporal lobes by adding a resection of the sphenoid greater and lesser wings to the middle fossa to achieve a resection of the superior orbit on the affected side only. They did not describe regarding sphenoid ridges. But the first author participated in the operation and actually saw the removal of the sphenoid ridge.
Referring to these historical findings of anterior cranial fossa anatomy and surgical procedures, we have performed bilateral frontal craniotomy, made an orbital bar, and resected the sphenoid greater and lesser wings, including overgrowth sphenoid ridge.
During orbital bar creation, a triangle was formed at the apex of the triangle considerably behind the orbital roof to the outermost and innermost edges of the supraorbital margin, because Hoffman et al. [11] pointed to occlusion of front-ethmoidal and front-sphenoidal sutures and, in some way, thought of releasing it close to these sutures. In infant cases, the frontal bone undergoes substantial bone deletion and is returned with a floating method. Marchac [15] describesd a case of CS in which bone regeneration occursed early in infancy, referring to a surgical procedure that iswas being performed in Europe. We have also performed significant bone deletions in our series, but we have not seen that the skull is resorbed or that the defect remains large.
In reports on development and intellect, while there are reports [1,2, 28] that treatment during infancy yielded better outcomes. Chieffo et al. [5] noted that in 35 infants, 7% of the cases of scaphocephaly biparietal cranial vault remodeling had visual memory impairment, 17% had attention deficits and other similar problems, while one-third of plagiocephaly cases were treated with frontal bone remolding and FOA, experiencing speech delay. Sidoti et al. [34] noted that there was impairment in 12 of 32 cases (mean age 6 months) including non-operated cases of trigonocephaly (11 cases). Kapp-Simon [14] reported impairment by elementary school in 47% of cases of trigonocephaly, scaphocephaly, and plagiocephaly operated in infancy, and Bottero et al. [3] reported impairment in 31.6% of cases with trigonocephaly. Thus, treatment in infancy is associated with a significant rate of disability.
In our cases that were treated in infancy, with the exception of one case of trigonocephaly, the long-term follow-up was uneventful, probably due to surgery involving the expansion of the frontal area and anterior cranial fossae as well as the unusually developed sphenoid ridges removal seen in all cases. Though the case of trigonocephaly also had a delayed medical examination with various impairments at the time of diagnosis before they received treatment, recovery has been observed postoperatively.
The abnormally developed sphenoid ridges that press the brain through the dura mater is called a sphenoid mirror brain (Fig. 7). It plays an important role in the development of children [6]. It has been discovered that mild trigonocephaly treatment has been performed, but the removal of the sphenoid ridge facilitates the recovery of this function [33].
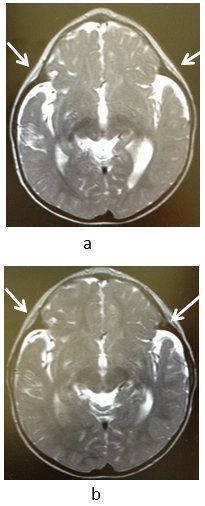
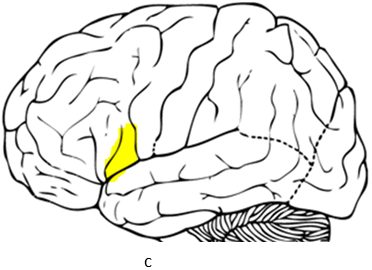
Fig. 7. The pars opercularis
A: Preoperatively, MRI showed that the pars opercularis (mirror neurons) was compressed (Table 1; 12).
B: Postoperatively, MRI showed that the compression at the pars opercularis (arrows) improved, allowing the frontal lobes to expand.
C: The pars opercularis (yellow).
All of our trigonocephaly cases were examined late. This causes a variety of disorders, as the cases suggest.
Typically, diagnosis is possible in early infancy, and familiarity with the pediatrician who becomes the first medical examiner is considered to be necessary.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.