Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Emily Ahn1*, Deanne Wilson-Costello2
1Neonatology Fellow, PGY-5 New York Presbyterian Weill Cornell
2Professor of Pediatrics, Director High Risk Follow-up UH Rainbow Babies and Children’s Hospital
*Corresponding author: Emily Ahn, Neonatology Fellow, PGY-5 New York Presbyterian Weill Cornell.
Received Date: January 07, 2022
Accepted Date: January 17, 2022
Published Date: January 19, 2022
Citation: Emily Ahn, Deanne Wilson-Costello (2022) “Parental Preparedness for NICU Morbidities in Parents of Extreme Preterm Infants: A Pilot Study.” Clinical Case Reports and Clinical Study, 7(2); DOI: http;//doi.org/01.2022/1.125.
Copyright: © 2022 Emily Ahn. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objectives: Assess which morbidities parents felt least prepared managing after discharge and measure parental perception of vulnerability.
Study Design: Fourteen parents of former extreme premature infants from a level four NICU were surveyed at the two year follow up visit. Questions were analyzed with Kruskal-Wallis one-way analysis of variance, and Dunn’s test. The Bonferroni correction was applied.
Results: Only 64% of parents felt prepared to care for their child after discharge, despite 93% feeling their infant was ready for discharge. Parents felt significantly more prepared to manage respiratory issues, medication administration, and communicating with multiple subspecialty teams compared to managing developmental delays, cognitive delays, and behavioral issues.
Parents were significantly more prepared to manage home oxygen than behavioral issues. Six parents of the nine medically stable children perceived their child currently as medically vulnerable.
Conclusions: Our data demonstrates gaps in NICU teaching subsequently indicating areas for improvement.
Introduction
Over the past few years the rate of NICU admissions has increased--growing from 64.0 per 1000 live births in 2006 to 77.9 per 1000 in 2012 [1]. At the same time, mortality has decreased from 14.0% in 2005 to 10.9% in 2014 [2]. Due to an increase in both admissions and surviving graduates, there are now more parents taking care of NICU graduates at home.
Lack of discharge readiness has been associated with worse outcomes and higher resource utilization. In mothers of term infants, lack of discharge readiness was associated with greater difficulty in coping with the care of their infant and twice as many phone calls to providers [3]. Another study showed a higher likelihood of emergency room or urgent care visits in the first month of life [4]. Specific to NICU graduates, a lack of discharge readiness was associated with an increase in feeding difficulties [5]. These negative outcomes may be improved by better preparing families for discharge and the potential needs of their neonate.
Multiple studies have focused on determining discharge readiness, [6-8] components necessary for discharge programs, [9] and these programs’ immediate effectiveness [10]. However, few have studied whether discharge and prenatal teachings have prepared parents long-term for common complications of a NICU graduate. The aim of this pilot study was to assess which specific problems parents felt least prepared for managing after discharge. The goal of this study is to use the data to refine NICU teaching, with the hope of improving the transition to home-going transition.
In addition to difficulties in transition of care, some parents struggle with perceiving their child as medically stable after discharge. Therefore, as a secondary goal of this study, we assessed parental perception of child vulnerability (PPCV) amongst the same parents. Increased PPCV can lead to Vulnerable Child Syndrome [11] which, originally described by Green and Solnit (1964), is a constellation of behavioral and physical symptoms in children associated with parents who perceive their child as medically vulnerable. This perception persists after a perceived life-threatening event even though the child is no longer medically vulnerable [12].
Higher PPCV is important to identify as it has been associated with an increased number of ED visits,[13] lower adaptive development,[14] and lower language scores [15]. Assessing the prevalence of increased PPCV can lead to better education for families, with an aim to improve outcomes and hospital utilization.
Methods
Participants
Parents of infants less than or equal to 28 weeks gestational age at birth and had received care at Rainbow Babies and Children’s Hospital, a level four NICU, were asked to participate.
Participants were recruited at the two-year premature follow up visit and informed consent obtained prior to survey administration.
Surveys and Analysis
Two surveys were utilized. The first was designed by the study team and broken down into two sections: general questions focused on discharge readiness and specific questions focused on preparedness to manage neonatal morbidities. General questions were multiple choice and open ended while specific questions utilized a 10-point Likert scale. Given the small sample size non-parametric testing was chosen. The Likert scale questions were analyzed with Kruskal-Wallis one-way analysis of variance for significance and Dunn’s test for pair-wise comparison. The Bonferroni correction was applied to determine the appropriate alpha (0.001) given multiple comparisons were made. Categories with an n less than 7 were not statistically analyzed.
The second survey administered was the validated Child Vulnerability Scale [14]. This is an eight-question survey containing a four-point multiple-choice response ranging from definitely false to definitely true. Answers were scored 0-3 with a possible total score range of 0-24. A score of 10 or higher was used as the cut-off to indicate high perceived vulnerability, as previously determined by Forsyth (1996).
Results
Fourteen parents were recruited for this study. Their former preterm children ranged in gestational age from 23-28 weeks with a mean birth weight of 720 grams. Six were female and eight male. Average hospital stay was 223 days. All neonates had developed bronchopulmonary dysplasia. The majority were discharged with oxygen (71%), an event monitor (79%), and more than two medications (57%) (Table 1).
Table 1. Baseline Characteristics of Neonates.
|
Characteristic |
no. (%) or mean ± SD |
|
Total Participants |
14 |
|
Gestational Age |
|
|
23 weeks |
3 (21) |
|
24 weeks |
7 (50) |
|
25 weeks |
2 (14) |
|
27 weeks |
1 (7) |
|
28 weeks |
1 (7) |
|
Sex |
|
|
Female |
6 (43) |
|
Male |
8 (57) |
|
Birth Weight in Grams |
720 ± 160 |
|
Total Days Hospitalized |
223 ± 143 |
|
Diagnoses |
|
|
BPD |
14 (100) |
|
Surgical NEC |
0 (0) |
|
Medical/Laser Treatment of ROP |
4 (29) |
|
Severe IVH |
5 (36) |
|
Failed Hearing Screen |
3 (21) |
|
Discharged with |
|
|
Oxygen |
10 (71) |
|
Monitor |
11 (79) |
|
Tracheostomy |
3 (21) |
|
Gastrostomy Tube |
6 (43) |
|
>2 medications |
8 (57) |
|
Bayley at 2 Years of Age |
|
|
Motor |
73.4 ± 16.8 |
|
Cognitive |
75.4 ± 13.9 |
|
Language |
74.7 ± 18.5 |
|
BPD = Bronchopulmonary dysplasia; NEC = Necrotizing enterocolitis; ROP = Retinopathy of Prematurity; IVH = Intraventricular Hemorrhage |
|
Survey one revealed that a majority of parents were concerned about development and behavior problems. When asked what they wish they had been told, all but one parent stated development or behavioral issues. When asked what occupies their time the most, the majority again stated development or behavioral issues. Only 64% of parents felt prepared to care for their child after leaving the NICU, despite 93% feeling that their infant was ready for discharge. Of the seven parents who received prenatal counseling, only 57% felt it prepared them for their child’s outcomes (Table 2).
Table 2. General Parental Preparedness Questions.
|
Questions |
No. (%, n) |
|
Currently most concerned about their child’s: |
|
|
Development/Growth |
10 (71, 14) |
|
Medical Problems |
0 (0, 14) |
|
Behavioral Problems |
4 (29, 14) |
|
Chances for Survival |
0 (0, 14) |
|
Feel prepared to care for child after leaving the NICU. |
9 (64, 14) |
|
Feel infant was ready for discharge when left the NICU. |
13 (93, 14) |
|
If provided home monitor/pulse oximeter, device provided reassurance. |
10 (83, 12) |
|
Received prenatal counseling. |
7 (50, 14) |
|
Prenatal counseling prepared caretaker for child’s outcomes. |
4 (57, 7) |
|
View their neonate the same as their other children. |
2 (25, 8) |
When asked about NICU morbidities, more than half of parents were aware that specific medical morbidities were a possibility, but less than half were aware that developmental delays and behavioral issues were a possibility. Parents scored medication administration highest and behavioral issues lowest in level of preparedness for management (Table 3). A statistical difference was found in level of preparedness to manage the various NICU morbidities (p = <0.001). Parents felt significantly more prepared to manage respiratory issues, medication administration, and communicating with multiple subspecialty teams compared to managing developmental delays, cognitive delays, and behavioral issues (p = < 0.001). Additionally, parents were significantly more prepared to manage home oxygen than behavioral issues (p = < 0.001).
Table 3. Caregiver’s Level of Preparedness in Caring for NICU Morbidities/Therapies.
|
Morbidity/Therapy |
Aware Diagnosis a Possibility no. (%) |
Neonate has the Diagnosis1 no. (%) |
How Prepared to Manage Diagnosis 2, 3 mean (range) |
|
Respiratory Issues |
13 (93) |
13 (93) |
7.9 (1-10) |
|
Home Oxygen |
12 (86) |
10 (71) |
8.1 (1-10) |
|
Tracheostomy |
8 (57) |
2 (14) |
8.5 (7-10)4 |
|
Seizures |
9 (64) |
0 (0) |
-4 |
|
Cerebral Palsy |
12 (86) |
2 (14) |
3 (3)4 |
|
Vision Impairment |
13 (93) |
1 (7) |
9 (9)4 |
|
Hearing Loss |
12 (86) |
3 (21) |
6 (3-9)4 |
|
Feeding Difficulties |
12 (86) |
11 (79) |
6.6 (1-10) |
|
Gastrostomy Tube |
9 (64) |
7 (50) |
8.0 (3-10) |
|
Developmental Delay |
6 (43) |
14 (100) |
3.6 (1-10) |
|
Cognitive Delay |
9 (64) |
13 (93) |
3.3 (1-10) |
|
Behavioral Issues |
5 (36) |
11 (79) |
2.7 (1-7) |
|
Medication Administration |
--- |
--- |
9.1 (8-10) |
|
Finding Support Groups |
--- |
--- |
6.2 (1-10) |
|
Communicating with multiple subspecialties |
--- |
--- |
7.8 (1-10) |
|
1 As reported by caregiver 2 Based on 10 point Likert scale 3 Parents answered only if neonate has the diagnosis 4 Sample size too small to analyze |
|||
All fourteen parents were administered the Child Vulnerability Scale. At the time of survey administration nine former premature children were classified as currently medically stable by the healthcare provider. Six parents of those nine children scored a 10 or greater indicating high perceived child vulnerability (Figure 1).
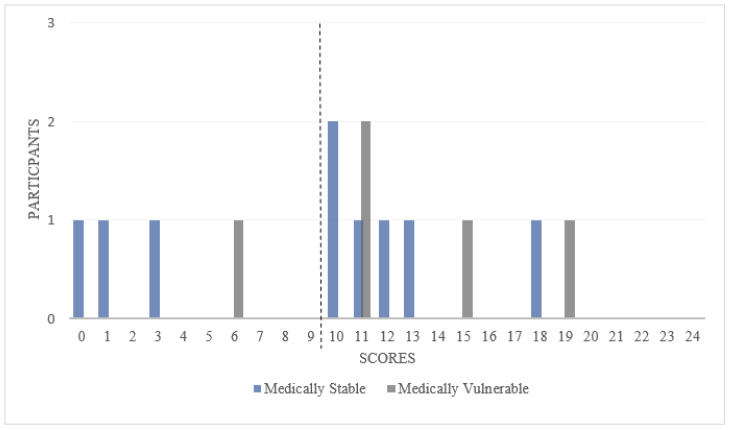
Figure 1. Participant scores of Child Vulnerability Scale. Scores greater or equal to 10 indicate 31 high vulnerability as perceived by the parent.
Discussion
Multiple studies have looked at both parental and infant discharge readiness from the NICU [6-9]. However, few studies have focused on assessing long term parental preparedness.
Through this pilot study we were able to demonstrate deficiencies in parental preparation in caring for a NICU graduate at two years of age.
Our data shows that our NICU teaching prepares parents well for medical morbidities.
Over half of parents were aware that various medical morbidities were a possibility for their infant.
Of those that had a medical morbidity, the mean score for preparedness was six or greater, with the exception of cerebral palsy. When parsing out the medical morbidities, parents generally felt more prepared for diagnoses that required hands on care in the hospital prior to discharge (home oxygen, tracheostomy care, gastrostomy tube care, and medication administration) than diagnoses without hands on experience (feeding difficulties and hearing loss). Given this, hands-on hospital care prior to discharge should be optimized. Some researchers are exploring simulation as a means of increasing hands-on experience [16].
Our data also shows that the majority of parents were unaware that developmental delay, cognitive delay, and behavioral issues were commonly associated with NICU graduates. Almost all infants were affected by one of these issues, yet the average score for preparedness ranged from 2.7 to 3.6, indicating an area for improvement in education. Delays, which are often seen after NICU discharge, are not always a focus of discharge teaching or not absorbed by NICU parents in the setting of learning how to manage medical complications. Therefore, connecting families post-discharge to early intervention, [17] parental support groups, and comprehensive care programs earlier and more frequently may help mitigate this issue.
In addition to addressing specific NICU morbidities or issues, many parents of former premature infants need to reframe how they view their child--from previously unstable to medically stable. Perceiving a medically stable child as medically vulnerable limits opportunities for the child through overprotection [18] and increases resource utilization [13]. Our study showed that parents struggled in perceiving their child as medically stable, indicating a need for continued education outside of the NICU period.
As a pilot study there are limitations when interpreting the data. The largest limitation is sample size as only fourteen parents were recruited. Given this limited cohort not all of the predetermined morbidities were represented as no infants in our study had seizures. Another limitation to this study is the population sampled. Only parents of extreme premature infants were offered participation, and extreme prematurity is only a portion of the NICU population.
Types and frequency of morbidities can vary based on gestational age. Therefore, education needed in this population may not apply to parents with neonates of older gestational ages.
Despite these limitations this pilot study has provided valuable information. It has demonstrated strengths and weaknesses in preparing parents to care for the NICU graduate, subsequently pointing to areas where education could be improved both prior to discharge and throughout outpatient follow up. Further research is needed in exploring the most effective ways in improving this education.
Acknowledgements
Angelina Williams for conducting tracking and contacting of patients.
Conflicts of Interest
The authors declare no conflict of interest.
Author Contributions
Emily Ahn, MD contributed in study design, data analysis, and manuscript writing.
Deanne Wilson-Costello, MD contributed in study design, administration of surveys, and manuscript editing.
Funding
Eunice Kennedy Shriver NICHD Cooperative Multicenter Neonatal Research Network funded the Bayley examinations.