Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Yasser Mubarak 1*, Hoda Mokhtar 2
1Cardiothoracic Surgery Department, Faculty of Medicine, Minia University, Egypt.
2Medical Oncology and Radiotherapy Department, Department, Faculty of Medicine, Minia University, Egypt.
*Corresponding author: Yasser Shaban Mubarak, MD. Assistant Professor of Cardiothoracic surgery, Minia University, Egypt.
Received Date: December 20, 2021
Accepted Date: January 10, 2022
Published Date: January 14, 2022
Citation: Mubarak Y, Mokhtar H, (2022) “Pulmonary Hamartoma in Breast Cancer Patient”. Clinical Case Reports and Clinical Study, 6(1); DOI: http;//doi.org/12.2022/1.124.
Copyright: © 2022 Yasser Shaban Mubarak. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Pulmonary hamartoma accounts for 77% of benign lung tumors and for 4% of all solitary lung nodules. Pulmonary hamartomas presented as a solitary peripheral mass 90%, and rarely multiple lesions. They are more common in adults, and their incidence in males is twice than in females. Objective: Pulmonary hamartomas are rare benign lung tumors and are composed of an abnormal mixture of epithelial and mesenchymal elements. They usually present as single, round nodules with distinct boundaries and are mostly asymptomatic. Case Report: We present a case of 47 years old female post bilateral mastectomy follow up period, who presented with cough, chest pain and dyspnea. Chest Computed tomography (CT) showed a well-defined non enhancing nodules measuring 3 × 2.5 cm and 1.5 × 1 cm seen in left lower lung lobe. Metastasis was differential diagnosis. Enclulation of two nodules was done through mini-thoracotomy. Histopathological examination confirmed the diagnosis of pulmonary hamartoma. Conclusion: It is common for confusion to occur when pulmonary nodules are found in the follow-up evaluation of patients who underwent mastectomy.
Introduction
Hamartoma was firstly described by Eugen in 1904. It is benign tumors that may occur in lungs, skin, heart, breast and other organs. Pulmonary hamartoma is the most common benign tumors in adults. It occurs more in male than females (1:4), in the 5th and 6th decade, with an incidence of 0.025 - 0.032%. Although, it is still an uncommon occurrence, it is the most common benign pulmonary tumor, about 77% of benign pulmonary nodules and 8% of solitary pulmonary lesions (SPN). It occurs mainly in the peripheral parenchyma. However, it is very rare in pediatric population, and endo-bronchial lesion. (1)
Most of pulmonary hamartomas are asymptomatic, and often being incidental discovered. Depending on its site and size, patients may develop symptoms; persistent coughing, wheezing, dyspnea. Endobronchial hamartoma may lead to airway obstruction, and manifested by hemoptysis, rhonchi, pneumonia, atelectasis or even pneumothorax. If it became symptomatic, fast-growing, and suspected malignancy cannot be excluded, surgical resection becomes necessary for diagnosis and treatment. (2) It is benign malformations of the lung and includes an abnormal mixture of tissue components; cartilage, epithelium, fat, and muscle. (2)
Surgical resection remains the curative option with excellent prognosis. Enucleation or wedge resections with preservation of lung parenchyma are the most common surgical choice. However, lobectomy or pneumonectomy indicated when lesion is deep, multiple, large, or adherent to the hilum. Pulmonary nodules that appear in mastectomy patients are usually pulmonary metastases and resection of pulmonary metastases (metastasectomy) is the treatment option. (3)
Case report
We present 47-years female asymptomatic patient referred from Oncology Department due to the presence of two pulmonary nodules discovered accidentally during follow up. She had a history of bilateral mastectomy (1-year apart) and axillary lymphadenectomy for invasive ductal breast carcinoma performed 3-years ago. The patient also had a history of hormonal therapy (20 mg/day of tamoxifen) and chemotherapy (cyclophosphamide + methotrexate + 5-fluorouracil: 4 neo-adjuvant cycles and 6 adjuvant cycles), as well as of adjuvant radiotherapy (total dose of 50 Grays for 5 weeks). She underwent chest computed tomography (CT), that revealed a two pulmonary nodules measuring approximately (3 × 2.5 cm) Figure (1)
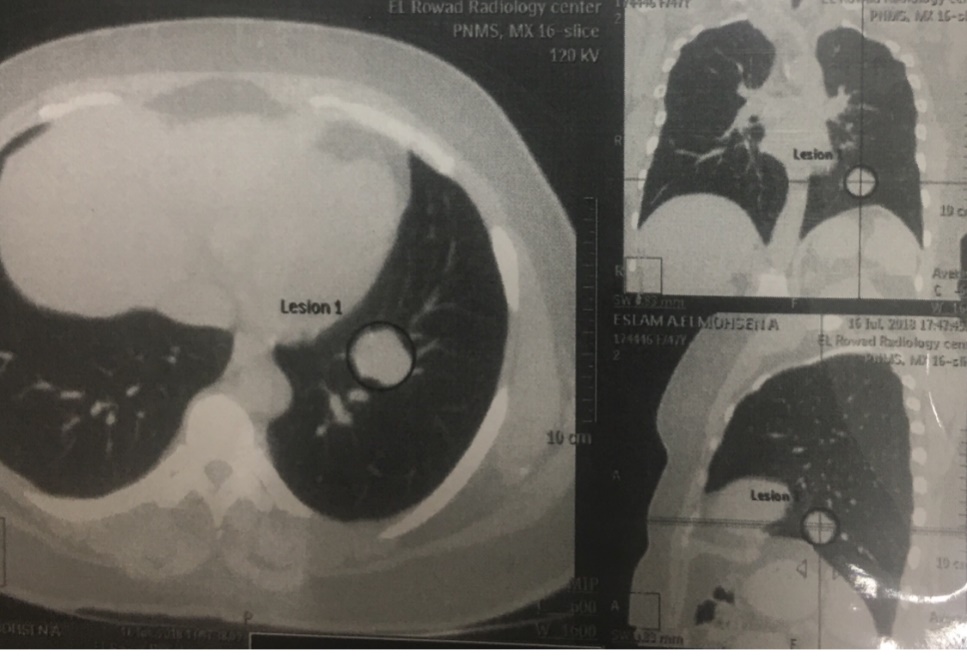
Figure 1: Chest CT showing pulmonary hamartoma in left lower lung lobe.
Therefore, pulmonary metastasis was the differential diagnosis and biopsy indicated for confirmation. Non-surgical diagnostic tools are controversial, very difficult and the surgery becomes unavoidable. Under general anesthesia, enucleation was performed through lateral mini-thoracotomy incision at the 5th intercostal space. After operation, pleura and lung parenchyma were examined for other nodules; also air leaks and bleeding were check. Patient was extubated at the operating table. The excised nodules were firm, and non-capsulated Figure (2).
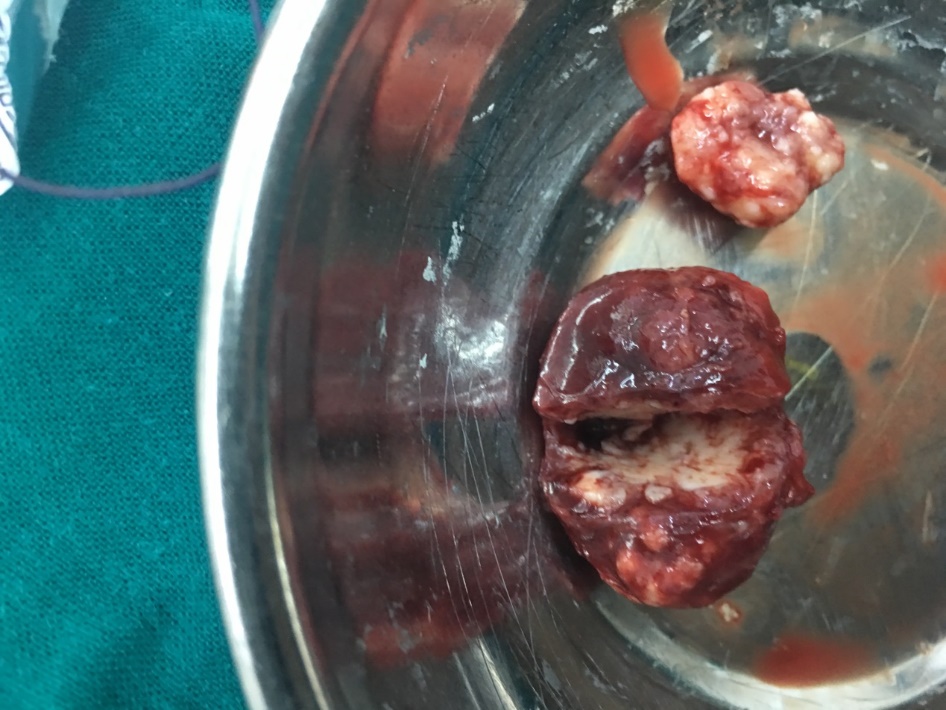
Figure 2: Photo illustrating the cut surface of the resected pulmonary hamartoma. The tumor was about 2 cm in the greatest dimension and was well circumscribed.
The patient recovered well and was discharged on 3rd postoperative day (POD). She is now under annual outpatient follow-up in Oncology Department, on hormonal therapy with tamoxifen for 3-years follow-up without tumor recurrence.
Discussion
The incidence of pulmonary hamartoma in the general population was 0.25%. It is more common in males than females (2-3:1), discovered during adulthood, and usually asymptomatic. (4) Pulmonary hamartoma mostly presents as solitary pulmonary nodule (SPN). (1) Nowadays, hamartomas are the third most common cause of SPN. (5) Surgical resection is a definitive diagnosis and treatment; also it is associated with a low incidence of morbidity and mortality risk. (1) Its treatment is usually conservative lung sparing surgery; wedge resection or enucleation of peripheral lesions. (4)
Pulmonary hamartoma is the most common benign tumors present in lungs and is often discovered accidentally with chest x-ray or CT. [5] Flu-deoxyglucose Positron Emission Tomography (FDG-PET) is useful for differentiation of pulmonary lesions. Pulmonary hamartomas show no or very mild metabolic activity. FNA biopsy is often inadequate because of dense fibrocartilaginous consistency of pulmonary hamartomas, and difficulties during aspirating adequate material. (1)
75% of patients, who undergo surgery for pulmonary nodules after mastectomy, present with lung metastases, 11.5% lung cancer, and 13.5% benign lesions, including hamartoma. Therefore, pulmonary nodules in breast cancer patients should be treated after pathological confirmation. One of the most common "symptoms" is fear, as these tumors can similar to cancer when found, especially on imaging. (5)
Conclusion
Pulmonary hamartomas frequently present as PSN. Surgical resection with preserving lung parenchyma is recommended for accurate diagnosis and treatment.
Abbreviations
CT: computed tomography, SOB: shortness of breath, POD: post-operative day, PET: positron emission tomography, SPSN: solitary peripheral nodule
Declarations
Ethics approval and consent to participate: - Patient confirms that have read and understood the information about the research as provided in the participant information sheet inside his file. Ethical committee approved that case report for publication. Patient signed agreement to participate the research, accepted to publish imaging from operation. The study conformed to the principles of “Declaration of Helsinki” and the investigator followed the appropriate safeguards regarding the rights and welfare of the human participants that have been included in the performed study. The formal approval and permission from our Cardiothoracic Surgery Department, Faculty of Medicine, Minia University was done.
Consent for publication: - It was obtained written consent from patients.
Availability of data and material: - It is available from recording files and data at cardiothoracic surgery department.
Declaration of Conflicting Interests: The authors declare that they have no conflict of interest.
Financial Disclosure: No financial support was received.