Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Todd Turner, William McEver*, Jack Xu, Asif Sewani, Hakan Paydak
Division of Cardiovascular Disease, University of Arkansas for Medical Sciences
*Corresponding author: William McEver, M Division of Cardiovascular Disease, University of Arkansas for Medical Sciences
Received: May 23, 2021
Accepted: May 30, 2021
Published: June 03, 2021
Citation: Todd Turner, William McEver, Jack Xu, Asif Sewani, Hakan Paydak “Pulmonary Vein Isolation Ablation As An Indirect Treatment For Torsades De Pointes”. Clinical Case Reports and Clinical Study, 3(4); DOI: 10.61148/2766-8614/JCCRCS/030
Copyright: © 2021 William McEver. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
QT prolongation is a known consequence when using antiarrhythmic drugs such as dofetilide to treat atrial fibrillation (AF). One potential complication of QT prolongation is the life-threatening arrhythmia Torsades de Pointes (TdP), but the prognosis for patients with an
acquired long QT syndrome is good if the offending agent is discontinued (1). We present a case in which pulmonary vein isolation (PVI) ablation successfully treated AF and, as a result, indirectly treated dofetilide induced QT prolongation by allowing the discontinuation of the causative agent.
We present a 59-year-old female with a history of non-ischemic cardiomyopathy with an implantable cardioverter-defibrillator (ICD) who presented with an episode of syncope.
Electrocardiogram (ECG) showed AF with rapid ventricular response. The patient failed rate control and was subsequently trialed on amiodarone, but it was stopped due to side effects. The patient was placed on dofetilide and underwent direct-current cardioversion via her ICD. She was subsequently discharged in normal sinus rhythm.
Eight days later, the patient returned to the hospital after experiencing nausea, palpitations, and light-headedness which resolved after a shock from her ICD. Electrocardiography in the ED showed an atrial-paced, ventricular-sensed rhythm at 80 BPM with new prolongation of the QT interval. The patient’s ICD was then interrogated and showed a non-sustained ventricular tachycardia that led to Torsades de Pointes (TdP). Dofetilide dosing was decreased upon admission and eventually switched to sotalol after echocardiography showed an improved ejection fraction of 37% from the patient’s previous 15%.
|
|
Figure 1: ECG showing a newly developed QT prolongation upon patient’s arrival to the ED after activation of her ICD in response to Torsades de Pointes.
After discharge the patient continued to have fatigue and palpitations associated with recurrent episodes of AF, despite medical therapy. Due to concerns of QT prolongation with an increased dose of dofetilide, we decided to proceed with pulmonary vein isolation (PVI).
One month later, the patient underwent a PVI as well as a right atrial cavotricuspid isthmus line ablation. During the procedure, she converted to sinus rhythm. Post-operative ECG demonstrated an atrial-paced rhythm conducting intrinsically. She was discharged the following day off of sotalol with clinic follow-up scheduled a month later.
At her follow-ups over the last five years, she remained in sinus rhythm. She reported feeling significantly better in terms of functional and respiratory status. On echocardiogram, her LVEF recovered to 55-60%.
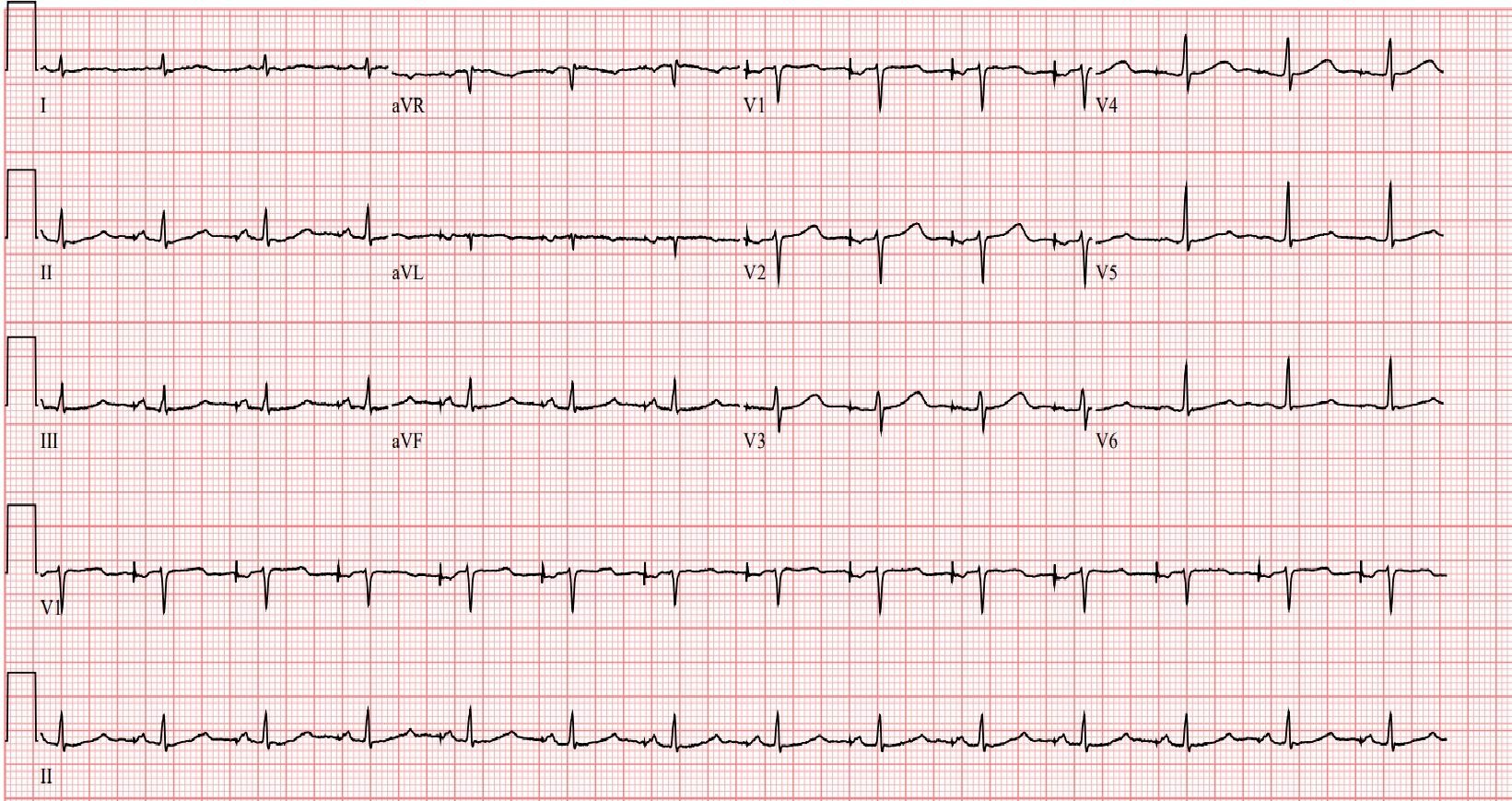
Figure 2: ECG showing normal sinus rhythm at discharge following patient’s PVI catheter ablation.
Treatment of AF can be quite complex in patients who remain symptomatic after initiation of rate controlling medications and must have antiarrhythmic drugs added to their regimen.
Amiodarone is a drug known to have numerous adverse effects and a significant number of patients simply can’t tolerate it despite its utility in rhythm control of AF (2). Alternatives such as dofetilide and sotalol, while they may have fewer side effects, carry a significant risk of QT prolongation and subsequent TdP(3). While there is limited research as to the exact incidence of TdP among the Class III arrhythmics, dofetilide has been reported in some studies to have an incidence of about 0.8-3.3% (4) and sotalol with an incidence of around 1-2% (3). There is also a risk in the use of amiodarone, but despite significant QT prolongation, amiodarone actually has a relatively small risk of progression to TdP(5). If patients subsequently develop QT prolongation, TdP, or are considered at high risk for developing Tdp due to past history or current medications, we propose catheter ablation as a potential therapy to both treat the AF and minimize the risk of developing TdP/QT prolongation. This would allow the immediate conversion of the patient from AF to normal sinus rhythm while also minimizing the risk of any further events of TdP that are caused by QTc prolonging agents. Our proposal is also in-line with the recently published EARLY-AF trial results (6).
While there have been several case reports of TdP after PVI and catheter ablation of AF(7,8), PVI ablation might be an effective treatment of AF and TdP in the setting of TdP secondary to QTc prolonging agents. Currently, there isn’t a lot of research on the incidence of QT prolongation when it occurs in the setting of PVI ablation, or if it is a transient event, nor is there sufficient data on the frequency of TdP after ablation to contraindicate its use. It appears, based on the available publications, that TdP is a more common phenomenon in the use of antiarrhythmic drugs than in the setting of catheter ablation for AF, however more research is needed for a more definitive answer.