Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Mahmoud Younis
Fellowship Trainer, Faculty of Medicine, Ain Shams University, Egypt
*Corresponding author: Mahmoud Younis, Fellowship Trainer, Faculty of Medicine, Ain Shams University, Egypt.
Received Date: December 09, 2021
Accepted Date: December 24, 2021
Published Date: January 07, 2022
Citation: Younis M, (2022) “Verapamil can be used as a Type 2 Diabetes Mellitus Saviour and Stopping the Need for Insulin in Uncontrolled type 2 Diabetes Mellitus”. Clinical Case Reports and Clinical Study, 6(1); DOI: http;//doi.org/12.2022/1.120.
Copyright: © 2022 Mahmoud Younis. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction:
Diabetes mellitus is not just a disease as it is already known, the matter is more complicated, and it is considered as an assembly of metabolic defects with end result of hyperglycemia.verapamil can decrease the expression of thioredoxin-interacting protein (TXNIP), which is recognized as an important factor in pancreatic beta cells.verapamil could enhance beta cell mass and function.
Materials and methods:
160 type 2 diabetes patients in 2 parallel groups.
Results: show statistically significant difference in favour of verapamil in increasing c-peptide levels and decreasing hba1c levels.
Conclusion:
Verapamil could be used as a type 2 diabetes saviour by increasing beta cell mass and function.
Introduction
Diabetes mellitus is not just a disease as it is already known, the matter is more complicated, it is considered as an assembly of metabolic defects with end result of hyperglycemia (1).Regarding chronicity, progressive course and probability of affecting all body systems, diabetes puts great impact on human health, affecting quality of life and increasing death ratio among patients (2).
Diabetes mellitus is not one type or one way disease, distinct subtypes resulting in defects in either insulin secretion or action (3).
Type 2 diabetes has the lion's share when compared with the other diabetes types as regarding incidence. As it represents more than 90 % of diabetes cases(4), and as it takes a progressive course , with time pancreatic beta cells can't secrete adequate and appropriate insulin for growing glucose demands. Beta cells which increase function early in response to stress emerging due to insulin resistance, with time can't afford these stresses giving rise to maladaptation and decreased function(5).For any disease to occur there is a culprit organ, culprit organ in diabetes mellitus is pancreatic beta cells but in partnership with the liver, skeletal muscles and adipose tissues(6).Also for type 2 diabetes to occur there must be an interaction between genetic factors and environmental factors with significant contribution of metabolic factors(7).A long time ago, it was considered that beta-cell death was responsible for type 2 diabetes ,this view has partially changed at the present time, as the term beta cell dysfunction is also frequently used to explain type 2 diabetes(8).In spite of many available oral drugs for treatment of type 2 diabetes, more than 60% of cases cannot be controlled . Making a need of external insulin in which even with it, a great proportion of patients cannot reach the glycemic goal (9).
Verapamil is an old drug approved by FDA for treatment of hypertension, angina and supraventricular tachycardia 40 years ago (10).
Recently, it is scientifically proven that verapamil can decrease the expression of thioredoxin-interacting protein (TXNIP), which is recognized as an important factor in pancreatic beta cells (11).It is discovered that (TXNIP) is increased in diabetic patients while its deficiency can prevent diabetes occurrence (12).It is also proven that (TXNIP) increase hepatic glucose production and decrease glucose uptake in peripheral cells (13).
By blocking l-type calcium channels, and decreasing free calcium in cells , verapamil can lead to (TXNIP) inhibition(14).It is well-known that pancreatic beta cells have high expression of calcium channels ,and so will get benefit of inhibition of txnip expression(15).
when using verapamil in patients with type 2 diabetes mellitus, inhibition of (TXNIP) expression may occur(16),with improving of beta cell function and increasing insulin production(17), also increasing insulin secretion(18).As it is known, (TXNIP)increase inflammatory markers, decreasing (TXNIP) may lead to anti inflammatory effects(19).Some studies suggested that verapamil could decrease type 2 diabetes incidence(20),also many studies suggested that verapamil could enhance beta cell mass and function(21).
Materials and methods:
160 type 2 diabetes mellitus and hypertensive patients into 2 parallel groups.
Each group had 80 patients, 50 males and 30 females. All patients were monitored in a private clinic. All the patients Lied between 30-60 years old. All patients are on maximum doses of glimepiride, sitagliptin, metformin and empagliflozin but are uncontrolled on this combination with hba1c more than 8.The first group received verapamil 240 mg as substitute or added to the present hypertension therapy for 6 months. The second group was still on hypertensive therapy but received lantus 20 units added to the oral therapy.
We measured hba1c and c-peptide levels in the 2 groups at the start of the trial and after 6 months of the trial.
Results:
For the analysis of data, we used an unpaired t-test.
t
Table 1: showing significant difference in hba1c before and after verapamil.

Figure1: showing significant difference in hba1c before and after verapamil.

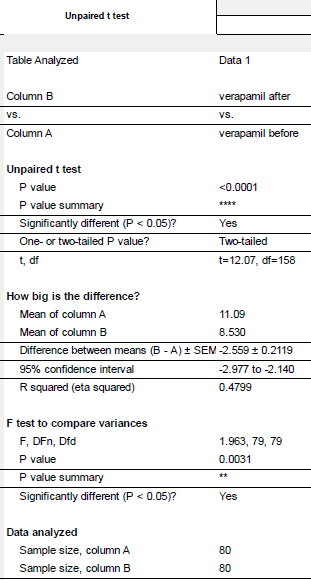
Table 2: showing significant difference in hba1c before and after insulin.
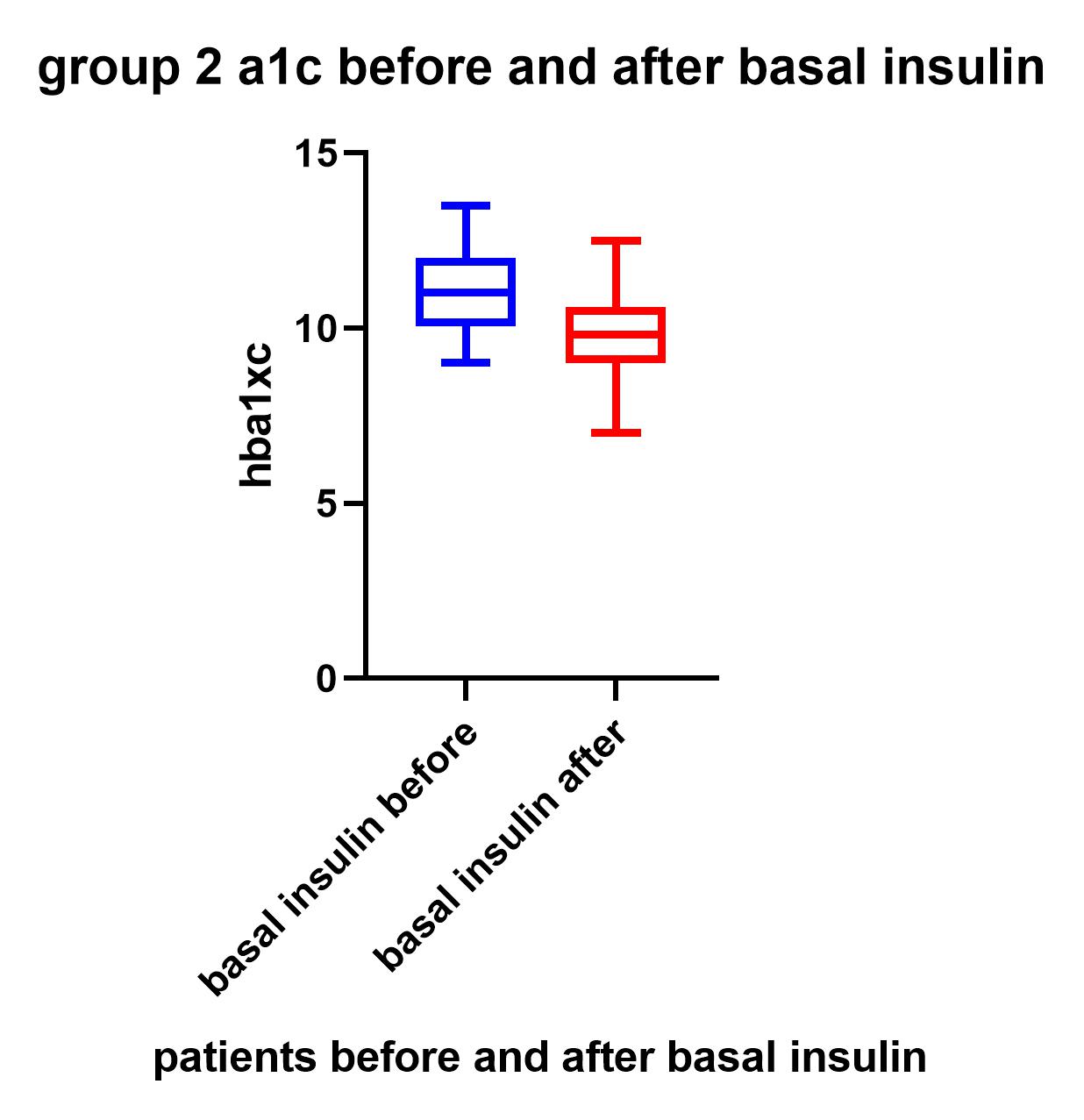
Figure 2: showing significant difference between hba1c before and after basal insulin
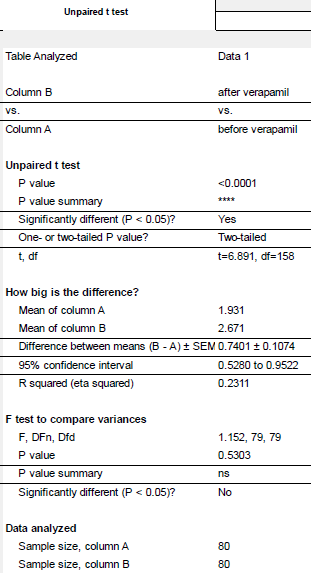
Table 3: showing significant difference between c-peptide before and after verapamil

Figure 3: showing significant differences in c-peptide before and after verapamil

Table 4: showing non significant difference in c-peptide before and after basal insulin.

Figure 4: showing non significant difference in c-peptide before and after basal insulin.

Table 5: showing significant differences between A1C after 6 months of treatment of verapamil vs. basal insulin.
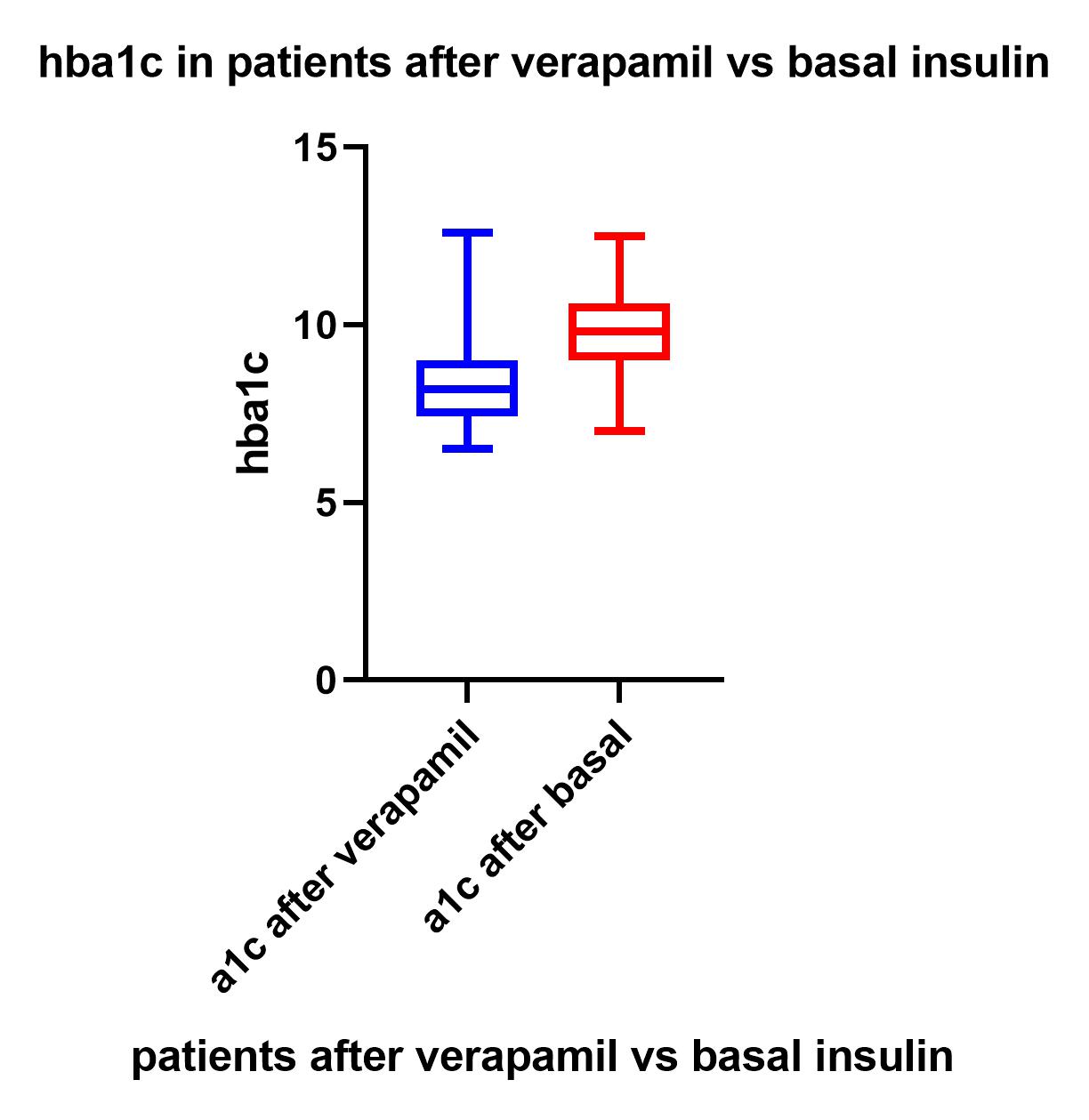
Figure 5: showing significant differences between A1C after 6 months of treatment of verapamil vs. basal insulin
The results show a statistically significant difference in hba1c in group 1 patients before and after 6 months of treatment with verapamil With p value less than 0.0001, as shown in table 1 and figure 1.The results show statistically significant difference in hba1c in group 2 patients with p value less than 0.0001 as shown in table 2 and fig 2. The results show significant differences in c-peptide levels in group 1 patients before and after 6 months of treatment of verapamil as shown in table 3 and fig 3. The results show non-significant differences in c-peptide levels in group 2 patients before and after 6 months treatment of basal insulin with b value 0.9822.The results show significant difference in hba1c after 6 months of treatment of verapamil vs. basal insulin with b value less than 0.0001.The results show that adding verapamil treatment is better than adding basal insulin in patients with uncontrolled type 2 diabetes on maximal oral treatment therapy. Results also show that verapamil can increase c-peptide levels after 6 months of treatment.
Discussion:
In Spite of advances in type 2 diabetes treatment and the discovery of new treatments which are based on physiological phenomena, type 2 diabetes mellitus is still a non curable and difficult to treat disease (22).And in most patients it is difficult to reach optimum blood glucose levels, even with optimal combination therapy with oral hypoglycemic drugs and even after adding or switching to insulin therapy (23). This may be due to the progressive course of the disease with progressive decrease in beta cell function and decreasing beta cell mass (24). Inability to reach control even with insulin therapy may be due insulin resistance to external insulin hindering its action, and the non physiological phenomena of external insulin (25).If we can enhance beta cell function, and increasing beta cell mass, this may lead to reaching optimal blood glucose levels and even may lead to diabetes remission (26).
Verapamil a drug approved for managing hypertension and angina(27), may be able to solve this problem by enhancing beta cell mass and consequently beta cell function which is detected by improved c- peptide levels and decreasing blood glucose levels, also verapamil could stop beta cell passing by decreasing (TXNIP) expression , a protein which leads to oxidative stress and apoptosis of beta cells(28).(TXNIP) is considered as a top glucose induced gene in beta cells and is considered as an important agent in beta cell apoptosis which is triggered off by by glucotoxicity(29).It must be considered that (TXNIP) expression may lead to beta cell dysfunction and inhibiting insulin synthesis(30). By using verapamil, a drug which inhibits (TXNIP) expression is valuable in improving beta cell function and preventing beta cell death and consequently decreasing blood glucose levels (31).
There are 2 limitations of this study; the first is the small number of patients but we can explore the results to the general population, the second limitation is whether the results are transient or persistent.
The results of our study show that verapamil could be considered as an option for treating type 2 diabetes. Further large-scale studies and clinical trials are needed to confirm our results.
Conclusion:
As type 2 diabetes is a progressive debilitating disease, with progressive decreasing of beta cell mass and function, and as it is difficult to reach target blood glucose in most type 2 diabetes patients, there is an urgent need to find a new drug to overcome this problem. Verapamil is a cheap FDA approved drug which is able to inhibit (TXNIP) expression in pancreatic beta cells. It is considered as a good option for enhancing beta cell function and could be used instead of insulin in uncontrolled type 2 diabetes mellitus with decreased beta cell function.
Data availability;
Data in supplementary information files
Conflicts of Interest
There is no conflict of interest to declare.
3- Kavya Chitra Mekala, Alain Gerald Bertoni,
Chapter 4 - Epidemiology of diabetes mellitus,
Editor(s): Giuseppe Orlando, Lorenzo Piemonti, Camillo Ricordi, Robert J. Stratta, Rainer W.G. Gruessner,Transplantation, Bioengineering, and Regeneration of the Endocrine Pancreas,Academic Press,2020.
4-Type 2 diabetes: principles of pathogenesis and therapy.
Stumvoll M, Goldstein BJ, van Haeften TW
Lancet. 2005 Apr 9-15; 365(9467):1333-46.
5-Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants.
NCD Risk Factor Collaboration (NCD-RisC).
Lancet. 2016 Apr 9; 387(10027):1513-1530.
Diabetes. 2009 Apr; 58(4):773-95.
Schellenberg ES, Dryden DM, Vandermeer B, Ha C, Korownyk C
Ann Intern Med. 2013 Oct 15; 159(8):543-51.
8-β-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment.
Diabetes Care. 2014 Jun; 37(6):1751-8.
10-Weaver-Agostoni J. Cluster headache. Am Fam Physician. 2013 Jul 15;88(2):122-8.
Chen J, Hui ST, Couto FM, Mungrue IN, Davis DB, Attie AD, Lusis AJ, Davis RA, Shalev A
FASEB J. 2008 Oct; 22(10):3581-94.
13-Adrian Po Zhu Li, Dulmini Kariyawasam, in Reference Module in Biomedical Sciences, 2021.
14-Preventing β-cell loss and diabetes with calcium channel blockers.
Xu G, Chen J, Jing G, Shalev A
Diabetes. 2012 Apr; 61(4):848-56.
Chen J, Cha-Molstad H, Szabo A, Shalev A
Am J Physiol Endocrinol Metab. 2009 May; 296(5):E1133-9.
16-Thioredoxin-interacting protein regulates insulin transcription through microRNA-204.
Xu G, Chen J, Jing G, Shalev A
Nat Med. 2013 Sep; 19(9):1141-6.
17-miR-204 Controls Glucagon-Like Peptide 1 Receptor Expression and Agonist Function.
Jo S, Chen J, Xu G, Grayson TB, Thielen LA, Shalev A
Diabetes. 2018 Feb; 67(2):256-264.
18-Thioredoxin-interacting protein links oxidative stress to inflammasome activation.
Zhou R, Tardivel A, Thorens B, Choi I, Tschopp J
Nat Immunol. 2010 Feb; 11(2):136-40.
19-Verapamil Use Is Associated With Reduction of Newly Diagnosed Diabetes Mellitus.
Yin T, Kuo SC, Chang YY, Chen YT, Wang KK
J Clin Endocrinol Metab. 2017 Jul 1; 102(7):2604-2610.
Am Heart J. 2006 May; 151(5):1072-9.
21-Preventing β-cell loss and diabetes with calcium channel blockers.
Xu G, Chen J, Jing G, Shalev A
Diabetes. 2012 Apr; 61(4):848-56.