Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Ricardo Gabriel Ascencio Tene1*, Verónica Michelle Ledesma Martínez2, Carmen Adriana Pérez Medina3, Rafael Camacho Cortés4, Ramón Sígala Arellano5, Claudia Margarita Ascencio Tene6, Héctor Raúl Pérez Gómez7
1Profesor-Investigador. Especialista en Medicina de Urgencias. Adscrito al servicio de Urgencias Adultos del Antiguo Hospital Civil de Guadalajara.
2Medico Residente de Segundo Año de la Especialidad en Patología Clínica.
3Medico Residente de Segundo Año de la Especialidad en Medicina de Urgencias.
4Médico Internista. Jefe de servicio de Urgencias Adultos.
5Patólogo Clínico. Jefe de Servicio de Patología Clínica.
6Oftalmóloga. Sub Especialista en Trasplantes de Cornea. Sub-directora de Enseñanza e Investigación
7Infectólogo. Director del OPD Hospitales Civiles de Guadalajara Institución donde se realizó: Antiguo Hospital Civil de Guadalajara Fray Antonio Alcalde
*Corresponding author: Ricardo Gabriel Ascencio Tene, Hospital 278, Col. El Retiro, Guadalajara, Jalisco.
Received: October 18, 2021
Accepted: October 23, 2021
Published: December 21, 2021
Citation: Ricardo Gabriel Ascencio Tene, Verónica Michelle Ledesma Martínez, Carmen Adriana Pérez Medina, Rafael Camacho Cortés, Ramón Sígala Arellano, Claudia Margarita Ascencio Tene, Héctor Raúl Pérez Gómez “Lipodystrophy - Can the radiologist give a clue to the diagnosis?.” Clinical Case Reports and Clinical Study, 5(4); DOI: 10.61148/2766-8614/JCCRCS/098
Copyright: © 2021 Ricardo Gabriel Ascencio Tene. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction: The diagnosis of acute myocardial infarction (AMI) in patients who have chest pain is difficult at times. Serum markers play an important role in the diagnosis of AMI when other indicators could be negative or questionable. The markers used in the diagnosis of infarction are creatine kinase (CK), MB isoenzyme of creatine kinase (CK-MB), myoglobin and troponin T and troponin I. Copeptin: is the C-terminal pro - vasopressin, a glycopeptide of 39 amino acids and a novel marker for rapid and reliable exclusion of AMI.
Objective: To evaluate the patient with chest pain in the adults emergency department triage and determine levels of Copeptin + Troponin at initial presentation to make better decisions based on reliable and accurate exclusion in patients with Ischemic Acute Coronary Syndrome (SICA) without ST-segment elevation / Unstable Angina (SE-SST / AI) in the Old Civil Hospital of Guadalajara "Fray Antonio Alcalde".
Methods: Study Design: Observational, analytical, prospective cohort study
Results: The point lower cutoff of 10 pmol / l copeptin has diagnostic performance with a sensitivity 23.7% (95% CI 10-37), specificity of 100%, a positive predictive value of 29% (95% CI 15-43), a negative predictive value of 100% a positive likelihood ratio of 1.31 (95% CI 1.1-1.56) and a negative likelihood ratio of 0. If we modify cutoff to 13 pmol / l sensitivity decreased to 91.7% with a specificity of 52.6%.
Conclusions: In the study population, the cutoff levels of copeptin that achieved the best negative predictive value for SICA (SE-SST / AI) was 10 (VPN 100%, specificity of 100% and a negative LR of 0). Unlike the cutoff point was considered to 6.6 pmol / l.
The importance of this biomarker lies in the ability to rule SICA (SE-SST / AI). The cutoff was 10 pmol / l for our population here was achieved discriminate the best diagnostic performance. Further studies with a larger order to confirm these results shows are required.
Introduction
Precordial pain is one of the reasons for consultation that most frequently requires medical attention. Each year in the United States 3 million people is hospitalized for evaluation of chest pain; From 2 to 8% of patients with Acute Myocardial Infarction (AMI) are discharged without diagnosis, these patients presenting twice the risk in terms of morbidity and mortality than those admitted and treated correctly, however between 40 -60% of patients admitted to hospitals do not have ischemic heart disease [1].
The diagnosis of acute myocardial infarction (AMI) in a patient with chest pain is difficult in many cases. The three main criteria indicated by the World Health Organization for the distinction between chest pain associated with AMI and chest pain due to other non-cardiac reasons are the following: 1) Anamnesis of the patient accompanied by a physical examination 2) Electrocardiographic data and 3) Changes in serum protein markers associated with myocardial infarction. To make a proper diagnosis of AMI, at least two of these 3 criteria must be met [2] Blood protein markers play an important role in the differential diagnosis of AMI when other indicators may be negative or questionable. The markers used in the diagnosis of myocardial infarction are: creatine kinase (CK), the isoenzyme MB of creatine kinase (CK-MB), myoglobin and the structural proteins of the Troponin complex, that is, Troponin T and Troponin I [3] Troponin is a constituent protein of myofibrillar muscle and was discovered in 1970, however cardiac troponin was isolated with radioimmunoassay and it was until 1980 that it was proposed as a specific marker of cardiac necrosis with high sensitivity compared to CK and CKMB [4].
Troponin as a Biomarker of choice in AMI was promoted in 2007 by the Word Heart Federation Task Force for the Redefinition of Myocardial Infarction [5].
However, recently a novel endogenous stress biomarker called Copeptin has been described, this molecule is also known as a Glycopeptide associated with the Arginine-Vasopressin system (AVP) which was described by Holwerda in 1972 [6]. Copeptin consists of a structure of 39 amino acids, which are glycosylated, and which contain a core segment rich in leucine. Together with AVP Copeptin is derived from a 164 amino acid precursor called pre-pro-vasopressin, which consists of an initial signal peptide, arginine vasopressin (AVP), Neurophysin II, and Copeptin [7].
Figure 1
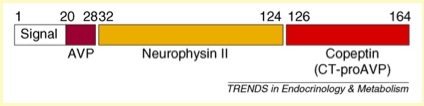
Copeptin is the C-terminal part of pro-AVP (CT-pro AVP).
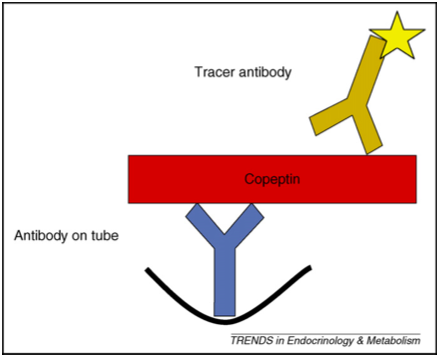
Recent tests on the measurement of Copeptin describe it as an immune-luminometric sandwich in which two polyclonal antibodies are used, one in the amino acid sequence 132-164 of the pre-pro-vasopressin of the C-region. terminal of the forerunner.
One anti-body is deposited in polystyrene tubes, and another is labeled with acridine ester for chemiluminescence detection, giving it great precision and dynamism. This assay offers considerable advantages over the measurement of the mature form of Arginine-Vasopressin (AVP) [8].
Figure 2
Copeptin as a Biomarker is a stress hormone of prognostic and discriminatory importance in the diagnosis, which is based on the positive correlation between the level of individual stress and the magnitude of the stressor or, in other words, the severity of the disease.
In addition, Copeptin is an easily measurable Biomarker that reflects the stress situation to which the body is subjected [9].
Copeptin is very useful in patients with chronic heart failure, the prognostic accuracy of Copeptin after an acute myocardial infarction is higher in patients who died or had a decompensation picture of chronic heart failure after an acute myocardial infarction which in patients surviving the event, therefore Copeptin is an independent predictor of death in heart failure [10].
The concomitant indication Troponin I - Copeptin, in the diagnosis of acute myocardial infarction results in high diagnostic precision, and under this reasoning this combination rules out AMI with a sensitivity of 98.8% and NPV of 99.7% [11]. Likewise, the determination of Copeptin in patients who come to the emergency department for chest pain and suspected acute coronary syndrome (AIS) is discriminatory, because Copeptin, as a stress hormone, is elevated in cases of cardiac ischemia and not in other conditions, which makes an excellent biomarker for decision-making in patients with suspected acute coronary syndrome [12].
Thus, Copeptin seems to be the ideal Biomarker together with Troponin to perform the rapid exclusion of AMI Vs Troponin alone, so that this would obviate the need for prolonged monitoring and serial determination of samples in most patients in the setting of health services. Emergencies [13].
Copeptin as a Biomarker to quickly rule out AMI in the emergency department in patients with chest pain <6hrs. has been studied according to the pre-test probability value of the test and it was concluded that in the triage of these patients the additional use of Copeptin + conventional Troponin (cTnI) allows a rapid exclusion of AMI despite any combination of pre-probability test that might exist to determine the accuracy of this conclusion [14].
The diagnostic role that Copeptin confers in patients with chest pain in the emergency room is that the measurements are not only used in the context of SICA, but in other life-threatening situations such as: Aortic Dissection, Pulmonary Embolism, Sepsis, and Pneumonia, this being an endogenous stress hormone that is generated in any of these situations.
Chest pain continues to be a diagnostic challenge for the emergency physician who must prescribe the use of Copeptin as a Biomarker when it is certain that the chest pain has a high probability of being of cardiac origin (family and personal history of SICA , clinical characteristics of pain and EKG) and / or there is also a high suspicion that it could be another situation that could endanger life such as those mentioned above, in order to assess the stress situation to which the patient is subjected organism in such a situation, with the limitation that the samples will have to be collected preferably in the first 8 hours after the onset of symptoms. In conclusion, this confirms that Copeptin confers a new strategy for patients presenting with chest pain of any origin to be evaluated in the emergency triage [15]. This is the reason why Copeptin has recently been listed among cardiac biomarkers by the National Academy of Clinical Chemistry [16].
The CHOPIN study (Copeptin Helps in the early detection Of Patients with acute myocardial INfarction) a multicenter study of 1,967 patients who presented to the emergency department to be evaluated for chest pain in the first 6 hrs of onset of symptoms, and where The objective was to demonstrate that Copeptin levels <14 pmol / l would allow a rapid exclusion of AMI when Troponin (cTnI) + non-diagnostic EKG was combined and In addition, the patients had a follow-up time of 180 days, which had not been reported in other studies, it determined that AMI (CE-SST and SE-SST) as a final diagnosis was presented in 7.9% of the patients studied (156 of 1967) confirmed with Gold Standard while> 60% had symptoms of non-cardiac origin. In contrast to current management guidelines for AMI where patients with undiagnosed chest pain + EKG should be observed for at least 3 to 6 hours or admitted to hospital to rule out AMI, CHOPIN demonstrated that negative Copeptin values (< 14 pmo / l) + negative cTnI, 58% ruled out an AMI, in all the patients studied with this characteristic, and who could also be discharged with certainty that they were not infarcted, since only 0.2% (n = 32 of 35 of 156) was likely to have a misdiagnosis. This led to a reduction in the delay time in decision-making by an average of 3 to 1.8 hours (43% reduction), assuming a delay of 3 hours in the second sample collection for analysis. However, the greatest benefit was observed in those patients with intermediate risk of AMI evaluated by the emergency physician, since a Copeptin value <14 pmol / l was compared with a risk subgroup that had a pre- low test for AMI. Thus, both tests were synergized.
Finally, CHOPIN is the first prospective cohort study designed with a pre-determined cohort point specifically to evaluate NPV in the exclusion of SE-SST AMI. This makes it a one-of-a-kind study. The study allowed to demonstrate that a negative value of Copeptin (<14 pmol / l) and a negative value of Troponin (cTnI) taken at the time of the presentation of the patient in the emergency triage, would allow to rule out an AMI with a NPV of 99% [17]. additionally, CHOPIN confirmed the predictive value of Copeptin alone as a predictor of death at 180 days of follow-up, which had been previously reported by Voors et al. And Kelly at all [18,19].
Currently there are original contributions whose objective was to evaluate ultrasensitive Copeptin (us-copeptin) in combination with ultrasensitive Troponin (hs-cTnT) in prospective studies that included patients who had initiated symptoms during the 12 hours prior to their inclusion. Of a total of 194 patients, AMI was found in n = 52 (27%), including SE-SST AMI n = 25 (13%), patients with AMI had higher levels of hs-cTpT and higher levels of us-copeptin, than those without AMI. However, the combination of both biomarkers improved the ROC curves (AUC) from 0.89 [0.85-0.92] to 0.93 for hs-cTnT alone [0.89-0.97]. Thus, the sensitivity and NPV increased particularly for SE-SST AMI (the diagnostic challenge in the emergency room) from 76% [54.9-90.6] to 96% [79.6% -99.9] and the NPV of 95% [90.4-98.3] to 98.9% [94.2 to 100). Thus, this study concludes that the evaluation of ultrasensitive Copeptin (us-copeptin) combined with high sensitivity Troponin (hs-TnT) at the time of admission to the emergency room allows us to safely rule out AMI, especially those SE-SST (without elevated blood pressure). ST segment) when they present negative results for both biomarkers [20].
Objective: To assess the patient with chest pain in the triage of the Adult Emergency service and determine Copeptin + Troponin levels upon admission, to make better decisions based on reliable and precise exclusion in the patient with Acute Ischemic Coronary Syndrome (SICA) without ST segment elevation / Unstable Angina (SE-SST / AI) in the Old Civil Hospital of Guadalajara “Fray Antonio Alcalde”.
Material and Method: Study Design: Observational, analytical, prospective cohort study.
Results
Table No. 1 contains the results obtained from the analysis of the set of variables that were studied and that presented some statistical significance or trend that supports the work described above. For its interpretation, the reasoning of the confrontation of risk variables Vs Percutaneous Coronary Angiography should be used since this continues to be the gold standard that serves for the diagnosis of ischemic heart disease of the AMI type.
Table 1
|
Resultado de la Angiografía para infarto agudo en el miocardio |
|||||
|
NEGATIVO |
valor de p |
POSITIVO |
valor de p |
||
|
HOMBRE |
21 |
0.516 |
8 |
0.248 |
|
|
MUJER |
17 |
4 |
|||
|
Diabetes tipo 2 |
|||||
|
Si |
73.9 (17) |
0.78 |
26.1 (6) |
0.75 |
|
|
No |
77.8 (21) |
22.2 (6) |
|||
|
Dislipidemia |
|||||
|
NO |
86.7 (26) |
0.009 |
13.3 (4) |
0.248 |
|
|
Si |
60 (12) |
40 (8) |
|||
|
Tabaquismo |
|||||
|
si |
50 (8) |
0.0001 |
50 (8) |
0.248 |
|
|
no |
88.2 (30) |
11.8 (4) |
|||
|
Edad |
|||||
|
59.1 ± 15.8 |
56.1 ± 8.7 |
0.538 |
|||
|
Horas en urgencias |
|||||
|
5.9 ± 2 |
5.9 ± 2 |
0.99 |
|||
|
Desenlace 24 hrs de seguimiento |
|||||
|
UCIC |
3 |
12 |
< 0.001 |
||
|
Piso Cardiología |
8 |
0 |
< 0.001 |
||
|
Alta de Urgencias |
27 |
0 |
< 0.001 |
||
|
Alcoholismo |
|||||
|
si |
100 (6) |
0.0001 |
0 (0) |
- |
|
|
no |
72.7 (32) |
27.3 (12) |
|||
|
IMC |
|||||
|
NORMAL <18.5-24.99 |
76.9 (10) |
0.014 |
23.1 (3) |
0.779 |
|
|
SOBREPESO >25-29.99 |
80.8 (21) |
19.2 (5) |
|||
|
OBESIDAD >30 |
63.6 (7) |
36.4 (4) |
|||
The cut-off point less than 10 pmol / l of Copeptin has a diagnostic performance with a sensitivity of 23.7% (95% CI 10-37), and a specificity of 100%, with a positive predictive value of 29% (95% CI 15 -43), a negative predictive value of 100%, a positive likelihood ratio of 1.31 (95% CI 1.1-1.56), and a negative likelihood ratio of 0.
Figure 3

Tabla 2
|
Área bajo la curva |
||||
|
Variables resultado de contraste: valor absoluto de la Copeptina para punto de corte menor de 10 |
||||
|
Área |
Error típ. |
Sig. asintótica |
Intervalo de confianza asintótico al 95% |
|
|
Límite inferior |
Límite superior |
|||
|
,776 |
,076 |
,004 |
,628 |
,925 |
Discussion:
Ischemic heart disease continues to be one of the main causes of mortality in Mexico and throughout the world. Ischemic heart disease encompasses a spectrum of diseases including acute coronary syndromes, with and without ST segment elevation on the EKG, and Unstable Anginas [21]. The diagnosis of SICA (acute coronary syndrome) was made according to the criteria set by the WHO (World Health Organization Expert Committee. Hypertension and coronary heart disease: classification and criteria for epidemiological studies. Technical report series number 168. Geneva: World Health Organization; 1959. In addition to current ESC management guidelines ( ESC for the management of acute coronary syndrome in patients without persistent ST segment elevation Working group for the management of acute coronary syndrome (ACS) in patients without persistent ST segment elevation of the European Society of Cardiology (ESC) Revista Española Cardiology 2012) For the determination of Copeptin blood samples were processed in a Thermo Scientific ™ BRAHM .S. ™ Copeptin KRYPTOR ™ in which automated immuno-fluorescent assays are processed for the determination of C-terminal pro Arginine Vasopressin (CT-proAVP Copeptin) in human serum, in tubes with heparin or with plasma EDTA. Rapid quantitative determination tests for Creatine Kinase MB (CK-MB) Myoglobin, Troponin I, BNP, and D-Dimer were performed with a Triage® Profiler SOB ™ Package Leaflet. According to our objectives, we selected patients with chest pain in the emergency triage, who had started their symptoms in the last 6 hours. And a baseline EKG was taken, sample collection to perform the Troponin test and Copeptin and those with a high suspicion of SICA were monitored in bed. To obtain the results of the coronary angiography, the patients were followed up for 24 hours. In the ICU (coronary intensive care unit). Finally, after crossing the study variables, we conclude that: 1) In our study, the male gender had a higher incidence of AMI than the female gender, which is compatible with what was reported by De'gano Elosua R, Marrugat J [22]. regarding Dyslipidemia and smoking as predictors of acute myocardial infarction were shown to have significant differences, increasing the risk of suffering an AMI if they are present at the time of patient evaluation. The outcome at 24 hrs showed that the patients admitted to the ICU surpassed the NO AMI, as reported in the literature [23]. However, one of our main findings is that the patients who underwent the Copeptin-Troponin test of Initially and is showing negative values as indicated in our results (Copeptin of 10 pmol / l / Troponin <0.05 pg / ml) they were discharged from the emergency room in a time of approximately 6 hrs, this makes the Copeptin test into an excellent discard marker, when its levels are below the cut-off point <10 pmol / l. To achieve the main objective in our study, the determination of a significant cut-off value (inflection point in the ROC curve) that achieved a sensitivity above 95% and a specificity close to 100% had to be achieved in the foreground. For which we had to adjust to find this inflection point, since for the Mexican population there are no reports in which absolute reliability + precision in laboratory tests can be had, where the cut-off value will find a NPV of 100%. This is contained in those previously reported by Maisel and Muller [24] and Camille Chenevier-Gobeaux [14]. Thus, this is one of our main strengths, since this clearly denotes that Copeptin as a biomarker of endogenous damage, could confer high sensitivity and specificity with high negative predictions (NPV), for detect an AMI in its early stages (first hours) by itself, increasing its predictive value when added to low troponin values, it could also serve as a predictor of death in the follow-up of patients at 180 days as reported by the CHOPIN study group17 and Voors et al. And Kelly at al [18,19].
Conclusions
In the present study, the cut-off points for Copeptin levels that achieved the best negative predictive value for acute myocardial infarction was 10 (NPV 100%, specificity of 100% and a negative RV of 0). Unlike the cut-off point that has been considered of 6.6 pmol / l. The importance of this Biomarker lies in its ability to rule out acute myocardial infarction in our population. The best diagnostic performance in this case was discriminated by having a cut-off point of 10 pmol / l.
Limitations: More studies with a larger sample are required to confirm these results.