Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Igor Klepikov
Pediatric Surgeon, 2116 27th St. NE Renton, WA, USA
*Corresponding author: Igor Klepikov, Pediatric Surgeon, 2116 27th St. NE Renton, WA, USA.
Received: September 01, 2021
Accepted: September 20, 2021
Published: September 24, 2021
Citation: Igor Klepikov. “The Myth of Septic Complications of Acute Pneumonia Clinical Case Reports and Clinical Study, 5(5); DOI: 10.61148/2766-8614/JCCRCS/090
Copyright: © 2021 Igor Klepikov. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A new era in the treatment of acute pneumonia (AP) began with the introduction of antibiotics into medical practice. The first successes of the use of new drugs were accompanied by a gradual simplification of views on the nature of AP with an emphasis on the characteristics of the pathogen and its suppression. A huge layer of scientific materials that allow us to understand the features of the development and course of inflammatory processes in the lungs, remained unclaimed. The focus on the etiology of the disease has led to a distorted view of its mechanisms and an exaggerated diagnosis of septic complications that do not have a reasoned confirmation. The current pandemic with a large number of COVID-19 pneumonias has radically changed the etiology of AP and deprived practical medicine of conventional treatment regimens. The unpreparedness of modern medicine for such a challenge and the preservation of the previous ideology of the disease are the reason for a radical revision of the AP doctrine.
Opinion and Perspective:
Bacterial sepsis and septic shock have for many years been considered the most severe complications and the main cause of death in patients with acute pneumonia (AP). Over the past couple of years, the number of patients with viral pneumonia has increased dramatically, but the frequency of septic complications, currently of viral etiology, actually remains the same [1,3]. The simplicity of determining the septic nature of these complications, which does not require microbiological confirmation, should raise doubts about the validity of such a statement, since the diagnosis sets the direction of therapeutic efforts and determines the final result.
In previous years, the peculiarity of the body's reaction to the inflammatory process was considered in the form of three main forms of manifestation of its reactivity: hypoergic, normoergic and hyperergic. That is, the previous gradation divided one of the characteristics of inflammatory diseases into possible individual variants from cases with a relatively slow and not always noticeable course of the process to the most aggressive and lightning-fast forms. Over a long period of antibiotic use, an exaggerated idea has developed about the leading role of the pathogen in the severity of clinical manifestations of AP. Such an interpretation of the disease clinic sets up in advance the expectation of septic complications in such patients. Currently, the concept of clinical manifestations of AP is based on the systemic inflammatory response syndrome (SIRS), indicating its clinical and laboratory criteria [4,6].
In the modern interpretation, the concept of SIRS in AP combines the body's reactions that do not go beyond the previous normoergic response. At the same time, low-symptomatic forms of the disease have actually ceased to be allocated to a separate group, and more severe manifestations of AP, depending on clinical and laboratory changes, are currently regarded as sepsis or septic shock [4]. The diagnosis of these complications in accordance with modern recommendations does not require such a cardinal confirmation of their septic nature as the detection of the pathogen in the blood. It is surprising that the etiology of the disease, which usually occupies the main place in the descriptions of AP, loses its significance just in those situations when it becomes a more important criterion.
In the literature on this issue, only isolated reports of bacterial forms of AP can be found, in which the frequency of detection of bacteria in the blood of patients with this disease is only from 10.7% to 12%, including not only cases of sepsis and septic shock, but also bacteremia [7,8]. The main reason for the negative results of bacteriological blood tests in most patients with sepsis and septic shock is the effect of preliminary antibacterial therapy [9,11]. The paradoxical nature of this conclusion is obvious, since it turns out that, on the one hand, antibiotics effectively destroy bacteria, but, on the other hand, they are not able to prevent "general blood poisoning".
The idea of the causes of the severity of clinical manifestations of AP should change dramatically if we remember the fundamental features of lung tissue damage. In modern publications, the mechanism accompanying inflammation in the lungs is not given due attention, so cases of sepsis and septic shock in patients with AP are not allocated to a separate group. The general material of the analysis of these complications usually includes information about various diseases in which patients with lung tissue inflammation account for up to 40-50% [6]. The combination of diseases with diametrically opposite pathogenetic mechanisms is a very serious misconception about such analytical work.
Even very scant information on the topic covered, which is presented above, gives reason for reflection and a thorough analysis of the validity of existing ideas. Such an examination will not bring full-fledged conclusions if we ignore a number of fundamental foundations of the AP. First of all, it is necessary to recall the general mechanisms of inflammatory transformation of tissues in the affected area.
There is no need to prove the fact that the basis of the pathological restructuring of tissue structures in the focus of acute inflammation is the indispensable development of a consistent reaction of blood vessels with a violation of blood flow in them and increased permeability of the walls. This transformation is also necessarily accompanied by five classic signs of inflammation: heat, pain, redness, swelling and loss of function. The last sign, a violation of the function of the affected organ, plays a leading role in the clinical manifestations and features of the disease.
But, the main feature of the topic under discussion is the fact that AP is the only inflammatory process that occurs in the small circle of blood circulation, unlike all other nosologies localized in the large circle. The inverse proportion of the functional state between the two circulatory circles with their inseparable anatomical and functional connection and interdependence underlies the fundamental differences between the pathological mechanisms of AP and inflammatory diseases of other localization. In this regard, the interpretation of the pathogenesis of AP by analogy with other forms of acute inflammation can in no way have the same scenario. The assessment of the detected deviations of blood flow parameters should also have a different interpretation.
The appearance of a focus of acute inflammation in the vessels of the small circle is a disaster for the body and the cause that disrupts the balance between the two halves of the circulatory system. The localization of this zone not only creates a physical obstacle to the main blood flow, which is ejected by the right half of the heart (see figure), but also is a source of reflex spasm of the pulmonary vessels [12,14]. The pressure in the vessels of the small circle begins to grow, and its throughput decreases. To correct this situation and avoid asynchronous operation of the cardiovascular system, which is incompatible with life, the body changes the parameters of the large circle of blood circulation, reducing the pressure in it and increasing its volume for a sudden "excess" of circulating blood (Schwiegk’s reflex).
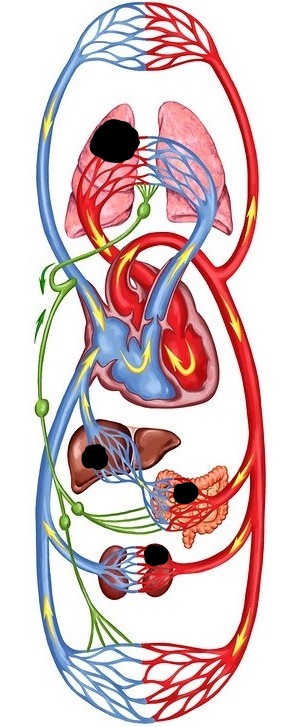
Figure 1: Schematic representation of the human circulatory system. The comparative value of foci of acute inflammation (black fields) for different organs and blood flow volumes, depending on the possible localization.
Autonomous regulation of blood circulation is one of the fundamental materials of medical science, and the described mechanism allows the body to avoid hemodynamic shifts in the AP that become incompatible with life. The more aggressive the inflammatory process develops, the less time the body has to adapt, and the more serious deviations are observed as a result. In such situations, the hyperergic reaction of the body to a sudden problem has long been considered as sepsis, although no evidence of the generalization of the infectious onset is given. In the most critical situations, secondary changes in peripheral hemodynamics fully correspond to the definition of shock, the origin of which is associated with damage to the pulmonary vessels and the body's attempt to restore the proportions between the two circles of blood circulation and the synchronicity of their work. This variant of shock is not caused by a septic factor, and it would be more correct to designate it as a pulmonal shock [15].
Incorrect interpretation of the cause of severe AP increases the concentration of attention on the etiology of the process in many cases without specifying a specific pathogen and leaves aside the true causes and mechanisms of critical situations. These misconceptions are further deepened as a result of existing approaches to assessing the condition of patients. The lesion of the vessels of the small circle is an indispensable result of inflammation of the lung tissue and the source of the resulting catastrophe of blood circulation. However, the idea of the septic nature of generalized circulatory disorders involves diagnosis, interpretation and their subsequent correction based on the parameters of peripheral blood flow. These principles, which are quite acceptable in other localities of the primary focus of inflammation, have the opposite meaning in patients with AP, when shifts in peripheral blood circulation are secondary and more reflect the adaptation process, rather than the initial manifestations of the disease.
The inverse relationship of blood pressure indicators in the small and large circles of blood circulation is well known, but the significance and role of this phenomenon in the pathogenesis of AP is not even mentioned today. Modern recommendations and protocols for the diagnosis and treatment of AP complications are focused on the leading role of etiology in the development and course of the disease. The cause and the beginning of this pathology is considered to be its causative agent, and the further dynamics of the process and its consequences are determined as a result of the aggressive properties of this cause. The existing principles allow us to widely use such diagnoses as" sepsis" and" septic shock", without resorting to bacteriological confirmation of these complications. The inviolability of this misconception continues to spread today to COVID-19 pneumonia. The severity of this form of the disease is explained by the development of viral sepsis and viral shock, which are considered as causes only by analogy with the existing concept of AP, without any objective evidence [1,3].
Widespread modern ideas about the nature of AP began to form after the introduction of antibiotics into medical practice. For many years, the treatment of this category of patients was defined as "antibiotics alone", creating a halo of the main problem of the disease around its pathogen. The desire to suppress the main cause of AP has narrowed and simplified the general view of the problem, leaving a huge layer of scientific materials unclaimed. Over the years, the etiotropic principle of AP treatment has turned into an endless search for a "pill for pneumonia", and most of the discussions on this problem have been devoted to finding, testing and comparing drugs that could act against the pathogen or its individual aggressive functions.
Although antibiotics have only the suppression of bacterial pathogens without directly affecting damaged tissues, they have played for many decades and still continue to play the role of the main treatment for acute inflammation in the lungs. The elimination of the inflammatory transformation of the organ and, most importantly, the restoration of its impaired function with such principles of treatment actually falls entirely on the compensatory and adaptive systems of the body. Additional medical care, which became more and more necessary over the years, was symptomatic, not pathogenetic in nature. The shortcomings of the existing concept of AP and the principles of its complex treatment have recently become quite obvious.
In the current SARS-CoV-2 pandemic, when a single agent spreads, there is an infinite range of clinical variants of infection, the diversity of which can no longer be explained, as before, only by the difference in pathogens. The priority of antibiotics has also become irrelevant in the treatment of COVID-19 pneumonia, and an equivalent replacement for this etiotropic therapy has not yet been found. However, the latter circumstance did not lead to a catastrophic increase in mortality from the coronavirus. According to dispassionate statistics, this indicator remains at the same figures as the mortality rate of recent years from bacterial forms of AP [6,16-23]. The reason for the identity of these indicators cannot go unnoticed, and its explanation requires an impartial analysis, since previously it was believed that patients with AP are treated at the level of maximum capabilities, and now we are talking only about auxiliary methods.
The facts of today's reality not only reflect the unpreparedness of modern medicine for the new features of the development of AP. The illusions about the universality and exceptional importance of antibiotics for the treatment process were destroyed by the counter-resistance of the microflora surrounding us. The negative biological consequences of prolonged antibacterial therapy have long been an undoubted fact and are well known. However, in recent years, another consequence of the sympathies and preferences of stencils for this type of medical care has become increasingly obvious. The instinctively established priority of antibiotics over other methods of AP treatment led to a negative didactic effect, which distorted ideas about the nature of the disease. These views dominate today and, contrary to the basic medical and biological canons, are accepted as the official truth in the last instance.
The latter circumstance is the main obstacle to solving the A P problem, which distorts our understanding of the essence of the task and shifts the emphasis when determining the research goal and ways to achieve it. In the context of the topic under discussion, further search for optimal solutions to the problem of AP requires recognition of existing conceptual misconceptions and a radical revision of the doctrine of the disease, where excessive diagnosis of septic complications of AP is only one of the links in the general system of distorted ideas [24,25].