Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Abdulrahman Hakami
College of Medicine, Jazan University, Jazan, Saudi Arabia.
*Corresponding author: Abdulrahman Hakami, College of Medicine, Jazan University, Jazan, Saudi Arabia.
Received: July 04, 2021
Accepted: July 10, 2021
Published: July 12, 2021
Citation: Abdulrahman Hakami “Imaging features with clinical correlation of COVID 19, A literature Review.”. Clinical Case Reports and Clinical Study, 4(4); DOI: 10.61148/2766-8614/JCCRCS/087
Copyright: © 2021 Abdulrahman Hakami. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
To date COVID-19 pandemic remains treatment challenge worldwide. Chest CT is an important tool in evaluation of COVID-19 and according to the literature, it has a high diagnostic sensitivity in diagnosis of COVID 19. The Typical imaging findings seen in PCR positive patients, Ground glass opacity and Consolidation. Mostly appeared in multiple lobes, particularly the basal part of lung. The atypical imaging findings such as pneumothorax, fibrosis, mediastinal lymphadenopathy, cavitation lesion and nodules, also seen in few cases.
Here we review comprehensively the correlated imaging finding, CT Chest and Chest X-ray with clinical picture in COVID 19 patients.
Abbreviation:
COVID 19 = coronavirus disease 2019, CT = computerized tomography, GGO = ground glass opacity.
Introduction
Coronavirus 2019 caused by a novel coronavirus which cause severe acute respiratory syndrome, COVID-19. It was first declared to the WHO on December 31, 2019 in Wuhan City, Hubei Territory, China (1,2,3,4,5). On March 11, 2020, the WHO announced COVID-19 a worldwide pandemic (6). Clinical manifestation of COVID-19 ranged from asymptomatic or mild to severe infection. The symptoms of COVD-19 usually occur between 2 days to 2 weeks following exposure to the virus either directly or indirectly (7). The median incubation period was 5.1 days, whereas 97.5% of patients developed the symptoms within 11.5 days of infection, this is according to a Chinese study, which included 181 patients with confirmed COVID-19 infection (8). Furthermore, Wu and colleagues studied a large number (n=72,314) of COVID-19 cases in China and found that 81 % have had mild pneumonia, 14% had severe pneumonia complicated with dyspnea and hypoxemia, while, 5% had critical illness characterized by shock, respiratory failure or multi-organ failure, overall mortality rate was 2.3% (9,10). According to the literature, the common symptoms of COVID-19 are fever (98%), tiredness (44%), dry cough (76%), dyspnea (21.9%), nasal congestion, sore throat or smell and taste loss (28%), nausea, vomiting and diarrhea (3.9%) generalized aches (8%) (11,12,13,14,15). Some COVID-19 patients reported gastrointestinal symptoms in a form of vomiting, diarrhea and abdominal pain and gastrointestinal symptoms might be the first presentation of the disease (16). Although few cases reported of acute hepatitis and liver injury consisting of elevation in serum bilirubin and liver enzymes mainly ALT, AST and GGT (17,18,19). However, the majority of COVID-19 induced hepatitis are mild. Few patients developed acute liver failure especially those with critical disease (17,19). The most serious manifestation of COVID-19 infection is pneumonia which is characterized by fever, cough, dyspnea and bilateral chest infiltrate on chest imaging (20,21). Old-aged patients with comorbidities are more prone to develop severe COVID-19 disease (9). Few patients developed severe COVID pneumonia while had no comorbidities (22). COVID-19 patients with severe disease usually require hospital admission and ICU care and has high fatality rate (23,24,25). The radiological abnormalities in COVID-19 can be detected using either chest x-ray or chest CT scan. The most common radiological abnormalities in COVID-19 are ground glass appearance and consolidation (figure 1 A, B). Consolidation is usually bilateral involving the lower lung zones and towards the periphery (figure 2 A, B, C, D) (26). The less common findings include pleural effusion, pneumothorax, lung cavitation, fibrosis, pleural thickening and hilar lymphadenopathy (figure 3 A, B, C, D) (27). In mild COVID-19 disease and before development of symptoms, the chest radiography might be quite normal (28). However, with progression of the disease the radiological findings will likely develop (figure 4 A, B) (29,30). On the other hand, radiological findings were detected in asymptomatic or pre-symptomatic adults with confirmed COVD -19 (31,32). RT-PCR test currently considered the gold standard for the diagnosis of COVID-19 (33,34). However, RT-PCR may yield a false-negative result in some cases, possibly because of inadequate viral material in the sample or technical issues during nucleic acid extraction (35). For these reasons, the recent clinical guidelines strongly recommend chest CT scan for patients with suspected COVID-19 (35,36,37).

CT chest (A) shows ground-glass exudation in both lungs, also bilateral consolidation in lower lobes as in (B).
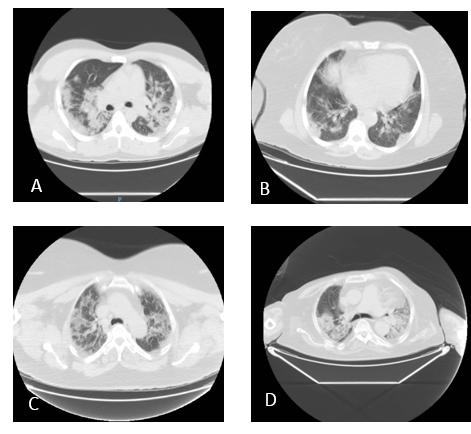
Bilateral multilobar subsegmental and peripherally subpleural ground glass opacities with consolidations in (A,B,C,D).
Objective:
The aim of this study is to present covid-19 cases who presented with typical radiological features and to provide an overview of existing literature on clinical and radiological manifestations of this disease.
Methodology:
A literature review comprehensively was carried out in online database search (PubMed, Google Scholar, Scopus and Web of Science) searching for articles submitted during COVID 19 pandemic, using the terms “Novel coronavirus2019”, COVID-19”, “SARS COVID-2” “Imaging, CT chest”.
An extensive manual search was performed for the referenced articles that concern with radiological role in diagnosis of COVID 19 and the clinical pictures of COVID 19.
The inclusion criteria were cross sectional studies, observational studies and retrospective or prospective studies.
Case reports, case-series, letters to editor and the preprint manuscripts that not peer reviewed were excluded, as well articles in non-English languages or those not related to COVID-19 not involved in this review.
Result:
Based on recent literature chest CT can play an important role in the early diagnosis and disease stratification of COVID-19 and this CT imaging not only helps in the diagnosis of the disease but also for other coexisted complications
Discussion:
The novel Coronavirus (SARS-COV-2), recently named as COVID 19, caused by β-coronavirus, a novel strain of coronavirus (2019-nCoV), similar to the previous two coronavirus outbreaks SARS-COV-1 and MERS-COV (2,4). This novel Coronavirus likely has a zoonotic origin, was first identified in Wuhan, in December 2019 and widespread human-to-human transmission has notified (2). Within a few months, the virus has spread from China and affecting 188 countries and territories around the world (38). On March 11, 2020, the World Health Organization (WHO) declared this global outbreak as a pandemic. Because the Coronavirus is highly contagious, the epidemic had spread worldwide and the number still increasing. Coronavirus Disease is an acute infectious disease that causes inflammation in the respiratory system and recently noted other systems can affected (12). The spectrum of this disease ranges from mild to severe, even life-threatening consequences (39,40). In a large cohort of patients with COVID-19, 81% had mild disease, 14% had severe disease, and 5% became critically ill with organ failure (39). The diagnosis of COVID-19 requires comprehensive consideration of exposure history, clinical manifestations, laboratory tests, and imaging examinations (40,41). The clinical diagnosis of COVID-19 is confirmed by the real-time reverse-transcription–polymerase-chain-reaction (RT-PCR) assay through combined oropharyngeal and nasopharyngeal swab samples. RT-PCR assay considered as the standard of diagnosis (11,12,39). Chest CT imaging is a conventional, non-invasive imaging with limited accuracy but recently in the observational studies reported with high sensitivity and specificity for diagnosis of COVID-19 (41,42,43).
Regarding the clinical findings, disease progression and treatment response can be monitored with serial CT examinations. According to the recent literature about COVID19, chest x-ray has low sensitivity, it can be widely used for monitoring the progression and later stages of COVID-19, especially in critical patients (figure 5 A, B) (43). Pulmonary ultrasonography instead of its lower cost, absence of radiation exposure, and the fact that it does not require sedation or transportation of unstable patients, but not used widely in COVID 19 outbreak due to limitation in sensitivity. The characteristic CT features, pattern of multifocal peripheral GGO, mixed GGO with predominance in the lower lung, with more extensive mixed opacity than GGO and bilateral multiple lobular and subsegmental areas of consolidation. Crazy-Paving pattern and reverse halo sign, cavities, enlarged mediastinal lymph nodes, or pleural effusions can present in advanced stage (45,46,47). In a retrospective analysis reported GGO were the most common CT manifestation and consolidation with fibrotic changes mostly found in severe and critical types of patients (48). The peak for lung abnormalities that are detected in patients with COVID-19 around 6-11 days after the onset of the symptoms (48,49). The improvement of CT findings appears around 14 days, the absorption stage may extend beyond 26 days (49). In another retrospective study fort 121 patients, reported the time between initial onset of symptoms and subsequent chest CT was known for 94 patients and assigned as early (0-2 days), intermediate (3-5 days), or late (6-12 days) (49). Those typical imaging features were also observed in patients with negative RT-PCR results but have clinical symptoms (50).
Therefore, in patients with negative RT-PCR tests or delay result, a combination of history, clinical symptoms, typical CT imaging features, and dynamic changes should be used to identify COVID-19 with higher sensitivity (36,37,51,52,53).
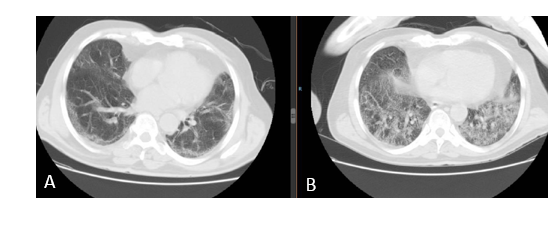
Chest X-ray for two COVID 19 patients in progressive stage in critical care, revealing bilateral infiltration in both lower lobes (A)(B).
Conclusion:
The imaging characteristics of COVID 19 has high sensitivity especially if correlated with clinical findings. CT chest is the best modality for imaging. The hallmarks imaging features are bilateral and peripheral ground glass with consolidative pulmonary opacities.
Source of funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not for- profit sectors.
Conflict of interest: The authors declare that they have no conflict of interest.
Ethical approval: not included in this article review.