Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Hakan Usta1, Yasin Kilic1, Ferhat Borulu1, Yavuzer Koza2, Umit Arslan1, Bilgehan Erkut1*
1Atatürk University, Medical Faculty, Department of Cardiovascular Surgery, Erzurum-Turkey
2Atatürk University, Medical Faculty, Department of Cardiology, Erzurum-Turkey
*Corresponding author: Bilgehan Erkut, Atatürk University Medical Faculty Department of Cardiovascular Surgery Erzurum, Turkey.
Received: May 20, 2021
Accepted: June 16, 2021
Published: June 24, 2021
Citation: Hakan Usta, Yasin Kilic, Ferhat Borulu, Yavuzer Koza, Umit Arslan, Bilgehan Erkut “Giant lymph node hyperplasia (Castleman's disease) in the retroperitoneal area”. Clinical Case Reports and Clinical Study, 4(4); DOI: 10.61148/2766-8614/JCCRCS/078
Copyright: © 2021 Bilgehan Erkut. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Castleman’s disease is a rare lymphoproliferative disease known as angiofollicular lymphoid hyperplasia. Castleman’s disease, which can be single or multi-center, is frequently detected randomly in asymptomatic cases, but may cause complaints according to the localization it originates from. Surgical excision is often curative in these cases that can only be diagnosed pathologically after detection. A 32-year-old female patient was admitted to the hospital with abdominal pain for 1 year, and computed tomography revealed a mass in the left lower abdomen at the level of the iliac arteries in the retroperitoneal area. The mass excision was performed in the patient who underwent laparotomy and a diagnosis of Hyaline-vascular type Castleman’s disease was made histopathologically. The possibility of Castleman’s disease should not be forgotten in masses detected in any part of the body, especially in patients with asymptomatic or vague symptoms.
Introduction
Castleman’s disease is a rare disease of unknown etiology, described by Castleman in 1956 and characterized by a large growth of lymphoid tissue (1). It is located mostly in thorax and mediastinum, especially seen in young woman. Although the most common location (70%) is the mediastinum, Castleman’s disease can occur anywhere in the lymphatic system. Extra-thoracic sites have been reported in the neck, axilla, pelvis and retroperitoneum. There are two forms. Hyaline vascular type (generally localized) and plasma cell type (generally multisentric). Hyaline vascular type consists of %90 of all cases. Plasma cell type is associated with clinical symptoms result from inflamatuary response. Hyaline vascular type is generally asymptomatic (2). Tissue diagnosis is mandatory to avoid mis-management,so surgical excision is a favorable approach for diagnosis and treatment in Castleman’s disease. Surgery is the optimal therapeutic approach only in the localized form, while for unresectable or disseminated disease, partial surgical resection, steroid, chemotherapy and radiotherapy have been employed with some measurable success.
Case Report
A 32-year-old woman applied to our hospital because of pain in the left lower abdomen for 1 year. Physical examination and other laboratory findings were normal. Lower extremity pulses were palpable manually. Ultrasonography was performed to investigate abdominal pain, and it was said that it could be lymph node enlargement, vascular malformation, or iliac artery aneurysm. However, computed tomography was performed because the diagnosis could not be made exactly. A computed tomography scan revealed a retroperitoneal mass approximately 10 x 12 cm in size located posterior and distal to the abdominal aortic bifurcation. The mass expanded and compressed the surrounding blood vessels as well as the bowels (Fig.1). However, it was decided to excise the mass surgically because it could not be distinguished whether it was lymphoma, vascular tumor, para-neurological tumor behind the psoas muscle, soft tissue tumor or hematoma. Since a definitive diagnosis could not be made by radiological examination, the patient was performed laparotomy under general anesthesia. The retroperitoneal area was opened and a giant mass approximately 10 cm in diameter was visible lateral to the left iliac artery. The mass was adhered to surrounding tissues, and compressing the iliac artery and vein. It was completely removed without any damage to the vascular structures (Fig.2). Peroperative or postoperative complications were not observed. In macroscopic pathological investigation, tissue samples were ovoid varying in size between 92x102 mm in largest dimension. Those were well circumscribed or even encapsulated. The out surface was homogeneous and grey-pink. Histopathologically, the structure of these tumour-like masses was the absence of lymph sinuses endosed by a well-defined fibrous capsuler and internal organization of the mass shows numerous follicle-like structures and a richly vascular interfollicular tissue. These follicules was usually small and their germinal center transfixed by radialy penetrating capillaries, often forming a characteristics “lollypop” structure (Fig. 3A and B). According to these histological data, it was diagnosed as hyaline - vasculer type Castleman’s disease. The patient was discharged on 9th postoperative day and she is now under observation.
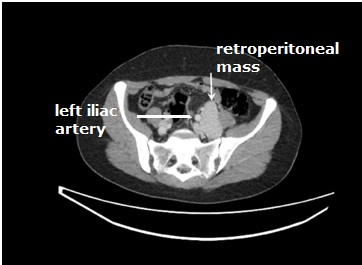
Fig.1. Computed tomography. Mass located in the left retroperitoneal area in the lower abdomen in the lateral posterior part of the left iliac artery, which cannot be diagnosed radiologically (arrow).

Fig.2. Surgically removed retroperitoneal mass approximately 10 cm in diameter
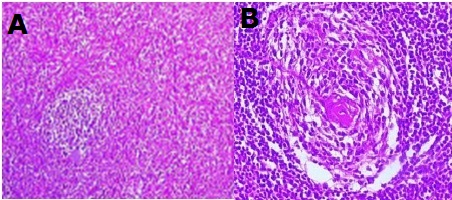
Fig.3A. Lymphoid lesion composed of numerous dispersed lymphoid follicles surrounded by a dense infiltrate of small lymphocytes (H&Ex 40).
Fig.3B. Small lymphoid follicules and their germinal center transfixed by radialy penetrating capillaries, often forming a characterictics “lollypop” structure (H and Ex200).
Discussion
Castleman’s disease, also known as angiofollicular lymph node hyperplasia, is a rare lymphoproliferative disorder that usually affects lymph nodes and, less commonly, non-nodal tissue. As seen in our case, most of the patients occur as a solitary mass, and it is most commonly localized in the mediastinum, abdomen, neck and axilla, retroperitoneum, mesentery and pelvis. Extranodal localized type of disease in larynx, thymus, lung, pericardium and vulva has also been described. Castleman’s disease has two types histopathologically. One of their is hyaline vascular, other is plasma cell type. Hyaline vascular type is generally localized while plasma cell type is multisentric (1,3). Unicentric disease is more common in the 3rd and 4th decade, whereas the multicentric form is more common in the 5th and 6th decade with no sex predilection. Diagnosis is usually based on histopathology features as imaging features show considerable overlap, thus posing diagnostic difficulties (4). Overall prognosis is good, particularly in the unicentric variety of disease.
Most patients are asymptomatic at diagnosis. However, in some cases, it may cause abdominal pain in intra-abdominal locations, as in our patients, and nonspecific complaints such as cough, shortness of breath, chest pain and back pain due to the tracheobronchial location of the mass. The hyaline vascular type frequently appears as a benign isolated mass and does not recur after curative surgical excision. Complete surgical resection is considered to be the gold standard treatment for unicentric Castleman disease, with an estimated 5-year overall survival rate of 98.4% (5,6). In contrast, multicentric Castleman disease has extensive lymphadenopathy affecting more than one group of lymph nodes with pronounced systemic inflammatory symptoms.
Although the etiology and pathogenesis of the disease are not fully known, different theories have been proposed including inflammatory, hamartomatous and mixed origin immune response. Recently, it has been reported that the disease may be associated with POEMS syndrome, paraneoplastic pemphigus, Hodgkin's disease, and follicular dendritic cell sarcoma. Many studies have determined that cases of Castleman disease are associated with Kaposi's sarcoma, human herpes virus-8 (HHV-8), and non-Hodgkin lymphoma, especially in its multicentric forms (3,4). No malignant change or association was detected in our patient.
Differential diagnosis of Castleman’s disease with many malignant and inflammatory diseases should be made (lymphoma, tuberculosis, sarcoidosis, fungal lymphadenopathy, sjogren's syndrome, pulmonary artery aneurysms, arterio-venous malformations, carcinoid tumor, Kaposi's sarcoma, metastasis, primary and secondary neoplasms). Abdominal forms are rare (10% to 17%), with the majority of cases being retroperitoneal. The four leading groups of diagnostic possibilities include mesenchymal soft tissue sarcoma, tumors of neurogenic origin, germ cell tumors, and lymphoproliferative disorders (2,4,6). Diagnosis is often made histopathologically after removal of the mass. As in our patient, the prognosis is generally good, especially in unicentric types, but the lesion should be followed up in case of recurrence.
Conclusions
Castleman disease should be taken into account when complaining of abdominal pain in a patient without any additional symptoms. In such patients, its presence should be investigated in ultrasonography performed for another purpose.
Acknowledgments
Consent
Written informed consent was obtained from the patient’s legal guardians/parents for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil
Funding
None
Ethical approval
Not applicable
Conflict of interest
The authors declare no conflict of interest
In this article the authors contribute equally