Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Arslan Ali Sohail1*, Karl Boyle2, Sharjeel Shaikh3
1MRCPI, Consultant physician Wexford General hospital, Former Stroke and Geriatric Registrar, Beaumont Hospital Stroke Service, Beaumont Hospital, Dublin
2FRCPI Consultant stroke physician Beaumont Hospital, Dublin
3Senior Staff Physician, Wexford General Hospital
*Corresponding author: Arslan Ali Sohail, MRCPI, Consultant physician Wexford General hospital, Former Stroke and Geriatric Registrar, Beaumont Hospital Stroke Service, Beaumont Hospital, Dublin.
Received: May 11, 2021
Accepted: May 19, 2021
Published: May 24, 2021
Citation: Arslan Ali Sohail, Karl Boyle, Sharjeel Shaikh “Tip of Basilar Syndrome in A Young Patient Treated with Tissue Plasminogen Activator”. Clinical Case Reports and Clinical Study, 4(1); DOI: 10.61148/2766-8614/JCCRCS/065
Copyright: © 2021 Arslan Ali Sohail. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background Tip-of-the-Basilar-artery-syndrome is manifestation of upper brainstem and diencephalic ischemia caused by occlusion of the rostral basilar artery
Case- We report a case of a 28 years old female who presented to her local General Hospital with confusion right ptosis, right INO and GCS of 7/15 diagnosed as tip of basilar syndrome and treated with IV TpA with good functional recovery
Discussion The case depicts the clinical signs and symptoms of a tip-of-basilar syndrome and, the importance of timely recanalization with IV TPA, which is shown to improve functional outcomes in acute basilar thrombosis
Learning Points
Importance of good history and establishing time of onset in acute basilar stroke, lead to better decision making and treatment offering
Identification of distinct clinical signs in acute stroke and, to establish their correlation with brain areas under and potential site of occlusion in acute basilar stroke.
Clinical signs of acute rostral basilar occlusion or tip of basilar syndrome
Importance of prompt and timely revascularization therapy in acute basilar occlusion, leading to improve outcome in an otherwise catastrophic stroke emergency with significant morbidity and mortality with delayed or no treatment
Case Report
History
e report a case of 28 years old female who presented to her local General Hospital with confusion, and GCS of 7/15. Patient was discovered by her Father to be in altered sensorium that morning. A selfie taken 14 mins before her discovery by her father, showed a right sided ptosis. The selfie also helped established her time of onset, as she remembered waking well prior to that, but then had no recollection of having taken the picture. Patient was therefore, brought in as acute Stroke call. Other examinations findings on arrival to Hospital were was a Right Inter-nuclear opthalmoplegia, Right ptosis, and GCS of 7/15.
Investigations
CT Brain showed a hyper-dense basilar artery and Digital subtraction angiography of circle of Willis and carotids showed non-opacification of her distal basilar and origin of both posterior cerebral arteries (Figure 1).
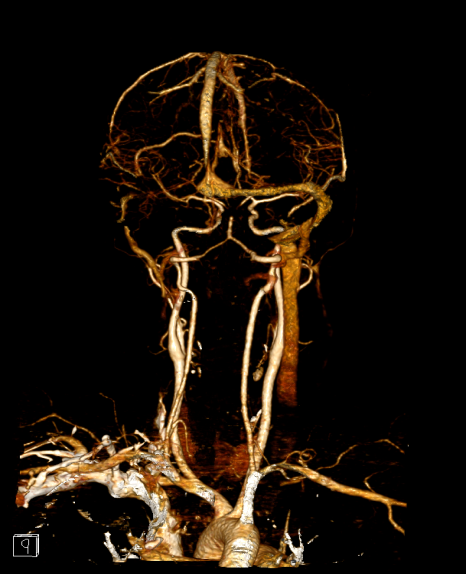
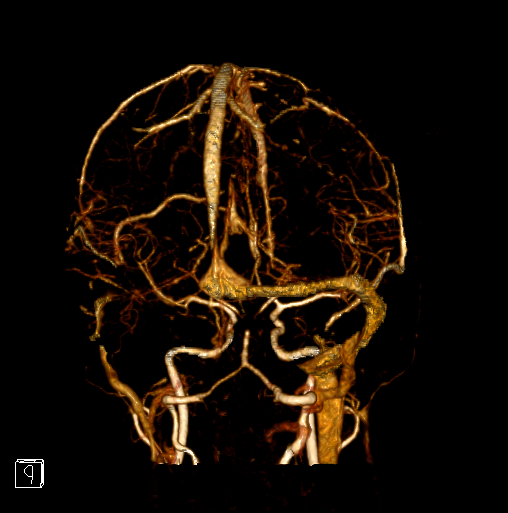
Figure 1A and 1B: Digital subtraction angiography reconstruction images showing non-opacification of distal basilar artery and bilateral post cerebral arteries’ origins (arrow)
Treatment and Further hospital course
Patient was treated with IV TpA 3 hours after established onset and was, referred for Endovascular thrombectomy. On arrival to thrombectomy centre, she had a emergent MRI which showed acute infarction in anterior left thalamus, median right thalamus, Right paramedian midbrain and R occipital lobe, which would explain her deficits in consciousness (thalamus), Internuclear opthalmoplegia and right ptosis(right paramedian midbrain). Her pons, medulla and cerebellum were spared which would be consistent with high/tip of basilar territory infarction (Figure 2). Her interventional angiogram showed full recanalization of her basilar artery. She was extubated in the next few hours and her NIHSS <12 hours post tpA, was 1. She made a great functional recovery. She was managed with dual antiplatelets therapy for 3 weeks followed by clopidogrel monotherapy. Her trans-oesophageal echocardiography revealed a Patent Foramen Ovale.


Figure 2A: (left) Diffusion weighed MRI showing acute infarction in right Para median midbrain (orange arrow) and left occipital lobe (blue arrow). Fig 2B (Right) showing infarction in R medial and left ant thalamus (arrows)
Outcome
On 3 month follow up, she maintains an mRS of 0 with a right residual INO and is awaiting, thrombophilia screen and PFO closure consideration
Summary/Discussion
Acute vertibulo-basilar thrombosis is associated with mortality of >85% mortality which is seen reduced to <40% with prompt recanalization. Good functional outcomes can be expected in as many as 24-35% of patients treated with IV or IA thrombolysis.
Tip-of-the-Basilar-artery-syndrome is manifestation of upper brainstem and diencephalic ischemia caused by occlusion of the rostral basilar artery. The most common cause is embolism. Common presentation is with altered sensorium, cranial nerve palsies, confusion and amnesia. Motor weakness is very rarely observed. The syndrome if unrecognized can lead to severe disability.
The case depicts very well the clinical signs and symptoms of a said syndrome with cranial nerve palsy, altered sensorium and amnesia and somewhat typical lack of motor weakness. It also emphasizes the importance of timely recanalization with IV TPA, which prevented severe brain stem damage in such a young patient and, the need for endovascular re-canalisation. The case re-enforces the limited yet present evidence that TPA in time, is shown to improve both immediate and long-term functional outcomes in acute basilar thrombosis. The vital importance of establishing time of onset via the most non-conventional means (patient’ own picture) proved substantive and indicated the importance of establishing correct time of onset in acute stroke and specifically in acute basilar strokes
Also the importance of good clinical history, examination and clinical correlation of neurological deficits with areas under threat their timely recognition with appropriate imaging improved outcome in this particular case
GLOSSARY/Index
IV/IA- Intravenous/Intra-arterial, GCS- Glasgow coma scale, CT- Computerized tomography, TpA- Tissue plasminogin activator, MRI- Magnetic resonance imaging, INO- Internuclear opthalmoplegia, DWI-Diffusion weight imaging, mRS-Modified Rankin Score.