Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Masato Kamimura, Hiroshi Sasaki*, Fumimasa Maruno
Department of Orthopedic Surgery, Kobe Rosai Hospital, Kobe, 651-0053, Japan
*Corresponding author: Hiroshi Sasaki, Department of Orthopedic Surgery, Kobe Rosai Hospital, Kobe, 651-0053, Japan
Received: April 09, 2021
Accepted: April 26, 2021
Published: April 29, 2021
Citation: Masato Kamimura, Hiroshi Sasaki, Fumimasa Maruno, “A Case Of Quadriceps Tendon Rupture With Osteophyte And An Avulsion Fracture Of A Patella Spur”. Clinical Case Reports and Clinical Study, 3(3); DOI: 10.61148/2766-8614/JCCRCS/051
Copyright: © 2021 Hiroshi Sasaki. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The quadriceps tendon is a strong structure that contributes to the knee extensor mechanism. Quadriceps tendon ruptures are quite infrequent because the structural and biomechanical properties of the normal quadriceps tendon can sustain very high loads. This injury most frequently occurs among middle-aged men who have some medical histories. Here, we report the case of a woman without an underlying medical history of quadriceps tendon rupture, who had osteophytes in the superior pole of the patella and an avulsion fracture of the patella spur. These osteophytes and avulsion fractures enabled prompt diagnosis and early surgical repair using anchors. Nine months postoperatively, the patient was able to dance and run. When the knee extensor mechanism is injured, osteophytes in the superior pole of the patella may be found in degenerative quadriceps tendons, and awareness of this may be helpful in the treatment of quadriceps tendon rupture.
1. Introduction
Rupture of the quadriceps tendon with an avulsion fracture of the superior pole of the patella is an uncommon, [1,2] disabling injury that requires prompt diagnosis and surgical repair [3]. The incidence of quadriceps tendon rupture is 1.37 per 100,000 individuals per year, and is more commonly reported among middle-aged males [1,4]. Degenerative changes associated with aging and calcific tendinopathy are also reportedly associated with quadriceps tendon rupture [5,6]. Metabolic disease, obesity, chronic renal failure, dialysis, and steroid use may alter the normal architecture of the quadriceps tendon via microscopic damage to the vascular supply, thus increasing susceptibility to rupture [7]. Here, we report a case of quadricep tendon rupture with osteophyte and an avulsion fracture of the patella spur in a woman without any underlying disease.
2. Case report
Informed consent was obtained from the patient for publication of this case report and accompanying images.
2.1 History and Physical Examination
A 74-year-old woman fell down after her right foot slipped, digging her foot into the road with her left knee in the flexed position. She experienced tenderness over the anterior portion of the knee and was unable to actively extend the knee but was capable of passive extension.
The patient had no relevant medical or family history. On examination, tenderness was observed over the suprapatellar region, as well as a large knee effusion. There was a palpable suprapatellar gap after arthrocentesis of the bloody fluid. The range of motion and lower limb diameters are shown in Table 1. Knee radiographs revealed osteophytes, avulsion fractures of the patella spur, and relative distal migration of the patella (Fig. 1). A knee computed tomography (CT) image also showed a patellar fracture fragment and osteophytes in the superior pole of the patella (Fig. 2). Magnetic resonance imaging (MRI) revealed complete disruption of the quadriceps tendon and osteophytes of the superior pole of the patella (Fig. 3).
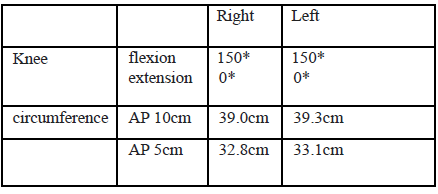
Table 1. Initial physical findings
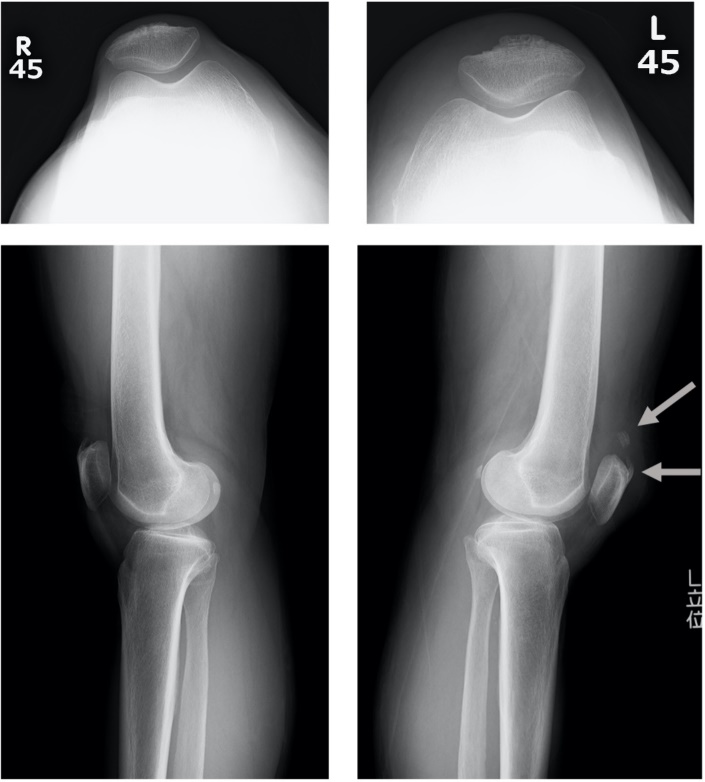
Figure 1: Lateral radiograph of the knee with quadriceps tendon rupture, shows the low position of the patella, suprapatellar avulsion fracture, osteophyte, and obliteration of the quadriceps tendon shadow (solid arrow)
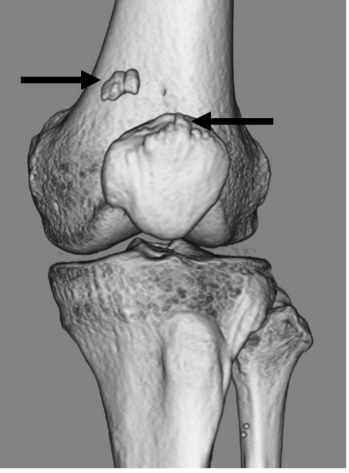
Figure 2: Computed tomography image of the knee demonstrates osteophyte and suprapatellar avulsion fracture patella spur (solid arrow).
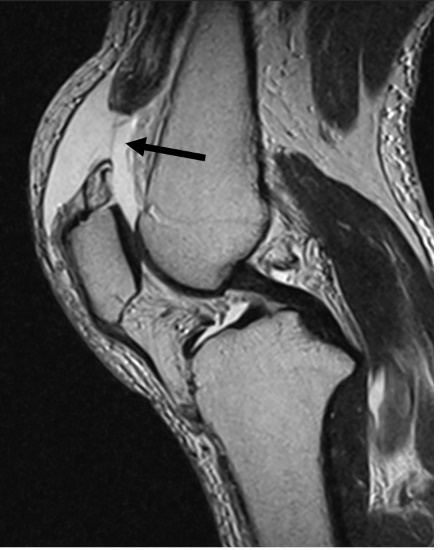
Figure 3: Magnetic resonance imaging (T2-weighted sagittal views) of the knee reveals a ruptured quadriceps tendon and hematoma (solid arrows)
2.2 Operation
Surgery was performed two weeks after the injury. A midline longitudinal skin incision was made and deepened to the level of the quadriceps tendon and the retinaculum. Dissection was performed to assess the full extent of tendon tears and to observe the superior pole of the patella. Upon inspection, complete rupture of the quadriceps tendon was observed, with a small bone fragment attached to the proximal tendinous rupture (Fig. 4a). Surgical repair was performed using suture anchor repair. The footprint of the superior pole was refreshed and decorticated. Two 5.5-mm double-loaded suture anchors (HEALICOIL® RG 5.5 mm; Smith and Nephew, Watford, Hertfordshire, UK) were inserted in the superior pole of the patella (Fig. 4b). These anchor holes were made on the patella and have been divided into almost equal thirds [8]. The anchors were then manually screwed in, remaining within the bone, and positioned medially in the sagittal plane. The tendon itself was again sutured using the Krackow whipstitch technique through the osteo fragment and quadriceps tendon. For suture anchoring, the knee was placed in a slight flexion position (Fig. 4c). Patellar positioning, tracking, and tensioning of the extensor mechanism were evaluated before closure. Suture quality was checked through a stress test at 90°, and no problems were observed with patellar tracking.

Figure 4a: Rupture of the quadriceps tendon (proximal: quadriceps tendon, lateral: superior pole of the patella)

b. Two double-loaded suture anchors were inserted in the superior pole of the patella

c. Repair of the tendon was performed using the Krackow whipstitch technique
2.3 Postoperative management
The day after the surgery, walking with full weight bearing was allowed, as well as knee extension with the support of a knee brace. Rehabilitation of passive flexion was initiated on day four, with a target of 15° per week, reaching 90° by six weeks. Straight Leg Raising training was actively performed three weeks after surgery, and the knee brace was removed six weeks after surgery. Return to sports was permitted at six months.
During the last follow-up after nine months, the patient was able to dance and run. The range of motion and lower limb diameter on examination are shown in Table 2. No significant differences were observed, and there was no muscle atrophy (Table 2). Knee radiographs revealed that the suprapatellar gap had disappeared (Fig. 5). Moreover, MRI showed that the quadriceps tendon was repaired (Fig. 6).
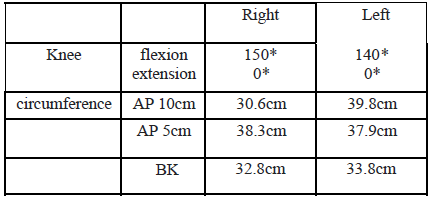
Table 2. Physical findings during last follow-up
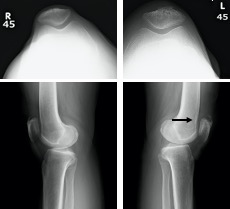
Figure 5: Lateral radiograph of the knee shows disappearance of the gap and normal position of the patella (solid arrow)
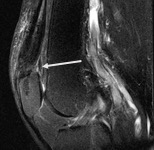
Figure 6: Magnetic resonance imaging (T2-weighted sagittal views) of the knee reveals that the quadriceps tendon was repaired using a suprapatellar anchor (solid arrow)
3. Discussion
Disruption of the extensor mechanism of the knee is rare [9], and is commonly caused by patellar fracture, patellar tendon rupture, and quadriceps tendon rupture. The quadriceps tendon is one of the strongest tendon fibers. Robert et al. reported that the incidence of quadriceps tendon rupture is 1.3% of various soft tissue injuries [10]. Therefore, quadriceps tendon rupture is often overlooked because it does not normally show up during radiographic examinations. Nevertheless, the radiographic appearance of a cranially displaced avulsed part of the patella should help in making a diagnosis of such a rupture. Hardy et al., reported that if it is as uncommon as a rupture of the quadriceps tendon, then the presence of a radiographically identified spur should alert the examining doctor to the possibility of such an injury among patients with traumatic failure of the extensor mechanism [11]. Prasad et al., reported a significantly higher incidence of patellar spurs among patients with quadricep tendon ruptures compared to those without [12].
There are several risk factors for quadricep tendon rupture. First, this rupture is more common among patients older than 40 years, who often have underlying medical conditions [13], and is eight times more common in men than in women [9]. Furthermore, indirect trauma is the most common cause of this kind of rupture among healthy people. In contrast, such ruptures can occur spontaneously in patients with predisposing factors, such as endocrine or rheumatic disease [14]. These diseases cause degenerative changes, such as fatty and cystic degeneration, myxoid degeneration, microangioblastic dysplasia, decreased collagen, and calcification, which naturally occur in tendons during aging. These findings suggest that it is necessary to search for an underlying medical condition in any patient presenting with a quadriceps tendon rupture. These changes alter the tendon’s architecture and may weaken it [14]. However, in our case, the patient was female and had no underlying medical conditions. She had osteophytes in the superior pole of the patella and an avulsion fracture of the patella spur. The appearance of osteophytes may hence be important for diagnosis in female patients without underlying disease.
Several surgical techniques have been reported for the repair of the quadriceps tendon. The most common sites of tears are located between 1–2 cm to the superior pole of the patella and, in older people, at the osteotendinous junction. Different techniques have been described and used to repair lesions without significant influence on the final outcomes [4]. One of the gold standard techniques for distal avulsion or rupture is reinsertion by transosseous patellar sutures [14, 15, 16]. Since the reports by Maniscalco et al. in 2000 [17] and Richards et al. in 2002 [18], anchors have been recommended for acute quadriceps tendon rupture. Suture anchor repair demonstrated a similar biomechanical profile with respect to cyclic loading and ultimate load to failure when compared with transosseous tunnel patellar tendon repair, with a trend toward less gapping in the suture anchor group [19]. Rougraff et al., [20] reviewed 53 ruptures performed through multiple surgical techniques and postoperative regimens and found no differences in clinical outcomes between multiple repair techniques or postoperative protocols. However, patients who have undergone delayed surgery had poor functional outcomes and decreased satisfaction scores. In our case, we repaired a quadriceps tendon containing a bone fragment of the patella using two anchors immediately after the injury. The patient returned to high-activity sports nine months postoperatively, and repair tendon fusion and patella alignment were also completely improved. We considered that good results were obtained by the repair with an anchor.
Regarding postoperative rehabilitation, Ronny et al., reported that early functional postoperative mobilization with full weight bearing after primary repair of a quadriceps tendon rupture is safe and does not lead to inferior clinical outcomes or an increased complication rate [21]. Quadriceps and patellar tendon repairs protected by a relaxing suture at a 30° knee flexion position are strong enough to safely permit early motion, weight bearing, and brace-free ambulation 4–6 weeks after surgery, while producing excellent results [22]. In our case, range of motion training and full load walking with a knee brace were started during physical therapy from the day after surgery, and brace-free ambulation was started six weeks after surgery. Therefore, it is possible that early range of motion training and loading will lead to good results after repair.
4. Conclusion
We presented a case of quadriceps tendon rupture in a female patient without any underlying disease. An osteophyte at the superior pole of the patella and an avulsion fracture of the patella spur enabled prompt diagnosis and early surgical repair using a suture anchor. Patella spurs may be observed in degenerative quadriceps tendons and may be helpful in the diagnosis and treatment of quadriceps tendon rupture.
Funding Sources
The authors declare no conflicts of interest associated with this manuscript.