Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Malaviarachchi S L 1, Balawardana J 1, Perera M 2, Senanayake A1, Perera R 1, Jayalath H 3
1 Sir John Kotelawala Defence University , Kandawala Road, Dehiwala -Mount Lavinia, Sri Lanka
2 Nevil Fernando Hospital , Malabe, Sri Lanka
3 Sir John Kotelawala Defence University Hospital, Werahera , Sri Lanka
*Corresponding authors: Malaviarachchi S L, Sir John Kotelawala Defence University , Kandawala Road, Dehiwala -Mount Lavinia, Sri Lanka.
Received: February 24, 2021
Accepted: March 23, 2021
Published: April 02, 2021
Citation: Malaviarachchi S L, Balawardana J, Perera M , Senanayake A, Perera R, “ Quting betel quid - A challenge to Reduce Head & Neck Cancer Incidence in Sri Lanka”. Clinical Case Reports and Clinical Study, 3(2); DOI:10.61148/2766-8614/JCCRCS/043
Copyright: © 2021 Malaviarachchi S L. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Squamous cell carcinoma of Head & Neck is the commonest cancer among males in Sri Lanka. [1] According to National cancer statistics in 2008 by National Cancer Controle Program (NCCP) ; lip oral cavity and pharynx cases were 1860 where as the second commonest among males were lung, trachea and bronchial tumours cancer incidence is 814; which is the second commonest cancer among males in Sri Lanka. According to world statistics in 2008; Head and neck cancers represent the sixth most common cancer with approximately 630,000 new patients diagnosed annually resulting in more than 350,000 deaths every year. [2] More than 90% of head and neck cancers are squamous cell carcinomas (HNSCC) that arise from the mucosal surfaces of the oral cavity.
Introduction
Squamous cell carcinoma of Head & Neck is the commonest cancer among males in Sri Lanka. [1] According to National cancer statistics in 2008 by National Cancer Controle Program (NCCP) ; lip oral cavity and pharynx cases were 1860 where as the second commonest among males were lung, trachea and bronchial tumours cancer incidence is 814; which is the second commonest cancer among males in Sri Lanka. According to world statistics in 2008; Head and neck cancers represent the sixth most common cancer with approximately 630,000 new patients diagnosed annually resulting in more than 350,000 deaths every year. [2] More than 90% of head and neck cancers are squamous cell carcinomas (HNSCC) that arise from the mucosal surfaces of the oral cavity.
HNSCCs has become the the eighth most common cancers worldwide after ten years (from 2008 - 2018) and account for 3% of all cancer diagnoses [3] However in south Asian area still the leading cancer is Head & Neck cancer [3] The incidence rate in males exceeds 20 per 100,000 in regions of Hong Kong, the Indian subcontinent, Central and Eastern Europe, Spain, Italy, and Brazil, and among African Americans in the United States. Mouth and tongue cancers are more common in the Indian subcontinent [4] According to Globocan 2020 total population in Sri Lanka is 21 413 250 and estimated Head & Neck cancer incidence is 2020 (15.6%) among males. Patterns of HNSCC incidence in Sri Lanka over the last 12 years from 2008 to 2020; there is no evidence of incidence reduction despite all the preventive measures taken by the relevant authorities Island wide. Tobacco smoking, alcohol, HPV and Ebstein bar virus are the commonest etiological factors identified [5]. According to Narayanhealth; 75% of head & neck cancers are due to tobacco and alcohol use. Smokeless tobacco, chewing or sniffing is recognised as another preventable risk factor for head & neck cancers.
Betel nut (BN), betel quid (BQ) and products derived from them are widely used as a socially acceptable masticatory product sincee ancient Sri Lanka. Meta-analysis done by Sharan [7] clearly points out the addictive nature of BN/BQ has resulted in its widespread usage making it the fourth most abused substance by humans. Progressively, several additives, including chewing tobacco, got added to simple BN preparations. This addictive practice has been shown to have strong etiological correlation with human susceptibility to cancer, particularly oral and oropharyngeal cancers.[7]
The Areca nut (AN), which is more commonly referred to as betel nut (BN) is masticated or chewed either alone or in combination with a wide variety of additives, which are often wrapped in the leaf of Piper betle popularly called as betel leaf. The name, betel quid (BQ) [8], name derives with name of Piper betal leaf which is freely growing as domestic and commercial plant in Sri Lanka.
The components of BQ can vary widely between countries, regions, communities and individuals. However, the major constituents are BN, catechu (Acacia catechu), a resinous extract from the wood of the Acacia tree, slaked lime, various additives, such as grated coconut, aniseed, pepper mint, cardamom, cloves, perfumes and stimulants wrapped in betel leaf. In Sri Lanka this is common among manual labourers, farmers, boutique keepers and drivers. The main objective of this study is to analyse the attitude on quitting BN & BQ chewing.
Several studies have reported the effect of BN and its constituents on human health, especially as a possible cause of oral cancer [9]
Methodology
This is a cross sectional descriptive study organised to commemorate world cancer day 4th February 2019 at Sir John Kotelawala Defence University. Samples were selected according to convenient sampling method. Total of 164 participants were participated as volunteers who wanted to quit BQ & BN were enrolled. The interviewer-based questionnaire was used to collect information regarding their attitude on quitting BQ & BN and data were analysed according to SPSS using X-el spread sheet.
Data Analysis
Interestingly all 164 volunteers were males and among them majority were between 20-40years. Only 13 were less than 20 years.( 18.3%) of total study population. Majority were from young adults (from20-40 years) 66 (40.2%) . Second significant representative group was from middle age population; 40-60years ;54 (32.9%). Among volunteers 28 were from 60-80 years age group and only 3were more than 80 years. 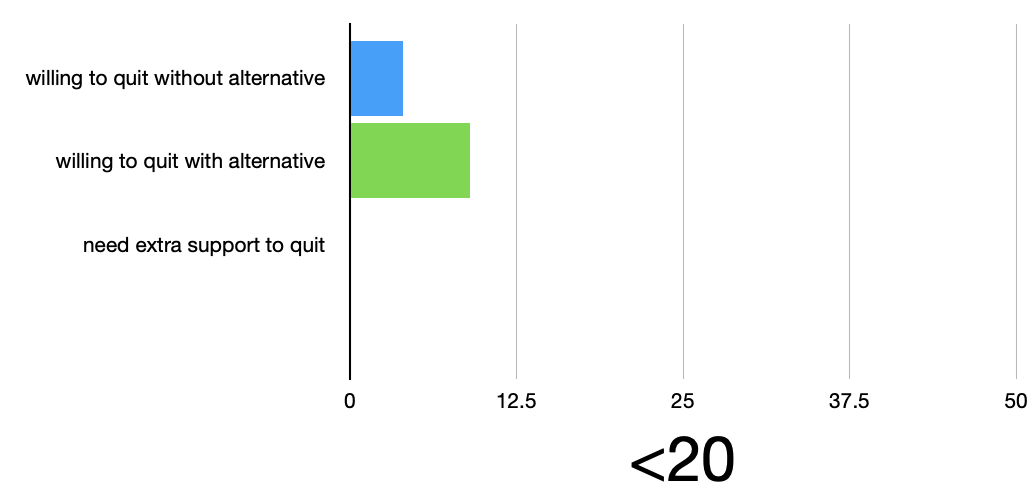
Figure 1: Different attitude on quitting BQ & BN chewing according to age
The reasons for BQ & BN chewing were very interesting and convincing. Sometimes this habit has been practicing since adolescence due to peer pressure. Majority wanted to quit the habit knowing that it is carcinogenic and they were psychologically bound or conditioned with their occupation. Most of their habits were acquired with the occupation. Especially drivers believe that the night time driving is easy with betal quid chewing while security workers believe their performance are sub optimal without BQ & BN chewing.
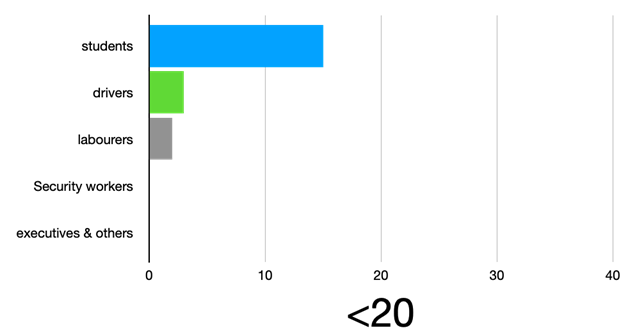
Figure 2: Type of occupation according to age groups
Among 164 volunteers who were willing to quit BQ & BN chewing; wide variety of occupants were there. Very interestingly those who wanted to quit BQ & BN chewing were drivers, labourers and security workers. Among volunteers in this study very few students and executives were there. There were many reasons for this addictive habit; most of the answers were ; as BQ & BN chewing arouse or induce feelings of pleasure and to feel more active during working especially drivers, labours and security guards.
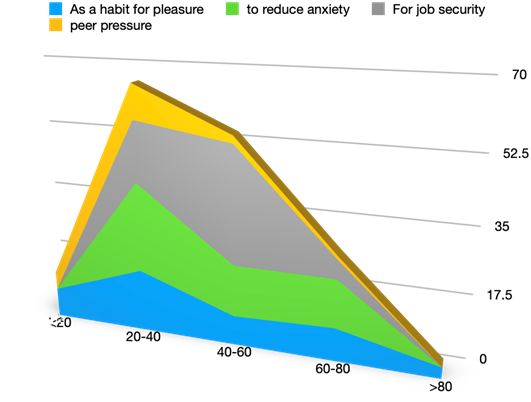
Figure 3: Reasons for betal quid chewing
Discussion
Research suggests that only 20–30% of drug users actually descend into addiction [10] It is defined as the persistent seeking and taking of the substance abuse even in the face of dire personal consequences. Although impulsivity is often seen as an effect of stimulant substance use, it may also be a causal factor in the loss of control that occurs when a substance abuser descends into addiction.
According to global cancer centre Michigen Medicine Quitting smokeless tobacco is like quitting smoking. [11] If someone use chew, snuff or pit tobacco making the decision to quit is similar harder as tobacco smoking. Those who are preparing to quit need set up goals. In this study we found that there were clear reasons for them to continue the habit of BQ & BN chewing. Most importantly when the need is reasonably link with their occupation what they requested was an alternative.
All the volunteers who participated in this study wanted to quit BQ & BN chewing because they have experience of known people suffering with oral cancers. According to international data; pharyngeal cancer incidence is significantly higher among the geographical distribution of habitats who used to have the habit of BQ & BN chewing since ancient era.
In evidence based practice it is obvious that if we can reduce the incidence of BQ & BN chewing the incidence of oropharyngeal cancer will be reduced. According to pubmed review [12] quitting smokeless tobacco is multitasking procedure. It includes set a goal or target date to quit and arrange regular followup under GP to make sure the compliance. Continuous health education regarding medical complications associate with quitting BQ & BN chewing.
According to this study; most users believe introducing alternative to chew during needy times is another very important supportive guid for quit BQ & BN chewing. Majority were willing to quit the habit of chewing BQ & BN if they have an alternative. Very few requested extra support other than the alternative.
In Sri Lanka there are various places that they can get extra support including psychiatry units in each general hospital and there are certain institutes who conduct especial programmes on cessation of smokeless tobacco such as National Authority on Tobacco & Alcohol(NATA) or National Cancer Controle Programme (NCCP) in Sri Lanka.
After this interview based study we propose that these programmes should be conducted at home based therapy by MOH areas. Involvement of community nurses, PHI and midwives are very important in supporting them with quitting BQ & BN chewing.
Conclusion
Reduction of head and neck cancer incidence in South East Asia is very important as it is the leading cancer among males in this region. The most importantly the incidence can be reduced with the reduction of risk exposure. BQ & BN chewing is a well recognised risk factor which can be minimised or reduced significantly with the implementation of well organised preventive measures at community level. Through this study we recognised it should be multidisciplinary task force including implementing continuous supervision of psychological aspect of addressing concerns that the individuals face during quitting BQ & BN. Majority believed; introducing safe alternative will be a very useful and practical approach to support them with quitting BQ & BN chewing.