Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Vijay Waman Dhakre 1, Prajesh Bhuta 2
1 Assistant Professor, Department of General Surgery, Lokmanya Tilak Municipal Medical College and General hospital, Sion, Mumbai, Maharashtra, India
2 Honorary Professor, Department of General Surgery, Lokmanya Tilak Municipal Medical College and General hospital, Sion, Mumbai, Maharashtra, India
2 Consultant Colorectal Surgeon, Department of Gastrointestinal surgery, Jaslok Hospital and Research Center, Pedder Road, Mumbai, Maharashtra, India.
*Corresponding authors: Vijay Waman Dhakre, Assistant Professor, Department of General Surgery, Lokmanya Tilak Municipal Medical College and General hospital, Sion, Mumbai, Maharashtra, India.
Received: March 15, 2021
Accepted: March 25, 2021
Published: April 02, 2021
Citation: Vijay Waman Dhakre, Prajesh Bhuta, “ Combined Abdominal and Transanal Approach for Managing Obstructive Defecation Syndrome with Internal Rectal Prolapse and Rectocele”. Clinical Case Reports and Clinical Study, 3(2); DOI: 10.61148/2766-8614/JCCRCS/042
Copyright: © 2021 Vijay Waman Dhakre. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Purpose: Obstructive-defecation syndrome (ODS) patients who have a large abdominal intussusception and an anal rectocele component may have an associated weakened perineum. In these patients, we feel that only a purely abdominal or transanal approach cannot tackle both the components and a combined approach may give us better results.
Method: We describe this combined approach in four patients. The abdominal approach was done laparoscopically. All patients had a ventral mesh rectopexy using a standard 3cm by 15cm polypropylene mesh. The perineal approach differed depending on the underlying clinical and radiological abnormality. One patient had a rectocele repaired transvaginally by the gynecologist, the second one had a transperineal repair with levatorplasty and in the other two male patients, and an internal Delorme’s procedure was done where there were a large rectocele and internal intussusception.
Results: One female patient had complete resolution of ODS in one-year follow-up but needs a small dose of laxative. The second patient had good evacuation on regular laxatives and good control. One of the male patients had an 80% symptom improvement with needing to spend 15-20 min in the toilet daily while the last patient had to continue to have some feeling of failure of evacuation 25% of the time. He needed the addition of mirtazapine for his bowel fixation.
Conclusion: The combined approach can be used to translate better outcome in a select group of people who have a combination of internal intussusception with rectocele, SRUS, poor perineal body, and a poor anal tone with prolapse.
Introduction:
Obstructive defecation syndrome (ODS) is a group of disorders leading to difficulty in evacuation with or without internal or external bowel prolapse. Patients generally complain of a sense of incomplete bowel evacuation. This may be accompanied by other symptoms like heaviness, self-digitation, bloating, and feeling to ‘go’ multiple times. It is most of the time associated with fragmented stools, tenesmus, mucus discharge, and/or a protruding mass [1,2,3,4,5,6].
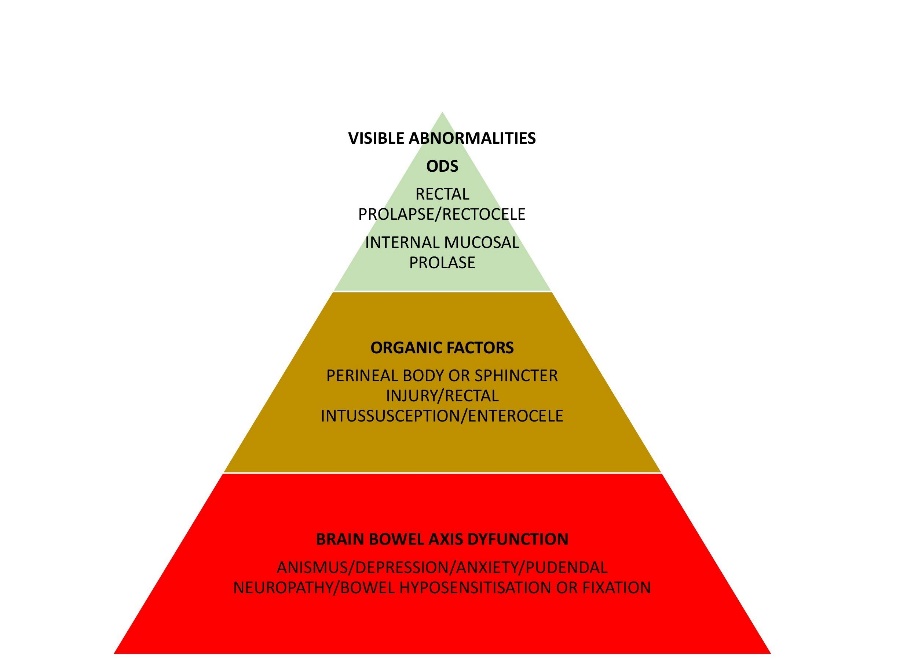
ODS an ‘iceberg syndrome’ was coined by Pescatori et al and is evaluated with the iceberg diagram for ODS. [2]. The surgical ship (procedure) sinks (fails) as it only tackles the ‘emerging rocks’ (rectocele / rectal internal mucosal prolapse) and ignores ‘underwater rocks’ (occult lesions) [1].
“To restore anatomy does not mean to restore function” - RI and rectal prolapse are seen upon the only condition that needs correction [Figure: 1] but it is most of the time the effect than the cause of the syndrome. [1,2,3].
Legends
Figure 1: Pyramid of cause and effect which leads towards Obstructive Defecation Syndrome.
ODS has shown to be a combination of three conditions and at least two occult conditions. [1, 2] Recurrence in long term is seen due to ignoring or not addressing these occult conditions. In patients seen at out pelvic floor OPD we have seen that most of the patients will have one or two symptoms of brain bowel axis dysfunction. These issues should be considered before planning surgery and surgical overtreatment should be avoided. An old Mayo clinic study showed that only 5% of patients with constipation will be benefited from surgery. After that many novel procedures have been attempted to provide better outcomes but we still don’t have an ideal or near-ideal procedure [1,2].
Surgeons for decades are using different procedures with variable success rates. But it becomes very important to evaluate all the aspects of ODS and tailor the surgical approach; as any mismatch between the two can lead to worsening of bowel function [5].
Procedure / Methods:
In all the patients the laparoscopic ventral mesh rectopexy (VMR) was common to take care of the intussusception component. Depending on the pathology and symptoms the perineal procedure differed as described below
Laparoscopic ventral mesh rectopexy (LVMR)
VMR has been suggested as a procedure that benefits patients with rectal intussusception with or without rectal prolapse by correcting the leading cause (the intussusception), preserving rectal innervation, and lifting the middle compartment, thus correcting coexisting enterocele or vaginal descent
Ports are inserted by the modified Hassan’s technique and in a head-down position; the small bowel is packed off. The sigmoid is put under traction, only the Denonvillier’s fascia is dissected to expose the anterior rectal wall and a single mesh is sutured onto the anterior aspect of the distal rectum. Posterior dissection is avoided and limited only to clearing the sacral promontory sufficiently for mesh fixation.
Using dilators in the vagina and rectum, the rectovaginal septum is splayed open and the peritoneum over the pouch of Douglas is excised to expose the anterior rectum. If asymptomatic rectocele or perineal descent is present, the dissection can be carried down to the perineal body and pubococcygeus muscles for additional support but because of the combined technique generally, this is not required.
A 5cm by 15cm mesh polypropylene mesh is used to fix to the anterior wall of the rectum by 2-0 ethibond and hitched at the other end to the sacral promontory by tackers. The rectum should not be placed under tension. The peritoneum is closed over the mesh completely.
Once this is done the perineal approach is started in the lithotomy position
Three types of surgeries are used in the combined approach depending on the symptoms and secondary abnormality.
If it is a large rectocele only with normal perineum we recommend only a rectocele repair transvaginally. If perineum is deficient along with a large rectocele we recommend levatorplasty and transperineal repair of rectocele
If the patient has SRUS with symptoms or with grade 3 intussusception we would add an internal Delorme’s procedure to the LVMR with excision of the SRUS.
Internal delormes procedure
The patient is in a lithotomy position with Allen’s stirrups and a PPH outer anoscope is fixed with silk so as to protect the dentate line, we take a circular incision of the mucosa at 2 cm proximal to the dentate line using monopolar electrocautery. Mucosal circumferential dissection from the rectal muscle layer proceeds proximally upwards for 4-5 cm until the surgeon can feel an increased resistance while keeping traction on the redundant mucosa. At the level of the resistance the mucosa is divided and the muscle is plicated longitudinally by eight 2-0 vicryl sutures. An interrupted mucomucosal suture completes the endorectal anastomosis. This was the approach adopted for two of the male patients one of whom who had an srus and the other a large rectocele
This combined approach treats not only the internal intussusception component of the ODS by LVMR but also deals with the perineal abnormalities like large rectocele, SRUS, and incontinence by tightening the perineum and correcting the defects.
Anterior pelvic floor repair
In case the perineum is weak with a deficient perineal body despite the abdominal VMR there will be poor perineum which will result in future recurrences of rectocele and symptoms. In these patients combining this anterior pelvic floor, the repair will not only take care of the internal prolapse but also correct the perineum. This may translate to fewer recurrences. During this procedure by a transperineal approach levatorplasty along with the creation of a new perineal body is done taking care not to go too deep so as to expose the mesh used in the LVMR.
This was adopted in one of our 65yr old patients who had an absent perineal body and perineal descent
Transvaginal rectocele repair
This is a very commonly performed procedure by the gynecologists and gives very good results for a large rectocele. If it’s a very low rectocele along with intussusception it is very difficult to correct with an abdominal approach alone and so patients with intussusception with a large low rectocele and ODS should benefit from this combined approach. This was done for one of the patients who had a normal perineum but a large rectocele.
Discussion:
Rectal intussusception (RI) /internal rectal prolapse (IRP) is seen in 50% of ODS. It is caused secondary to pelvic floor muscle disorders and neuropathy [1,2,3,4,5,6].
In this group of patients, we see maximum squeeze pressures, lower mean pressures, absence or malfunctioning rectoanal inhibitory reflexes, and lower rectal capacities. RI with even > 1cm can show manometric profile similar to full-thickness rectal prolapse and the defecography accuracy increases from 66% if RI is >3cm to 83% if RI is intrarectal [4].
Even though only 20% of ODS patient needs surgery their treatment should not be delayed more than 4-years as it is a high risk for recurrence postoperatively due to loss of pelvic floor muscles [1,7].
The main goals of the surgical plan must be to eliminate the prolapse by resection and or restoration of normal anatomy, correction of functional anomalies like constipation/incontinence, and avoid recurrence and new postoperative bowel dysfunction [7].
The most common approaches are transabdominal or transperineal. The transabdominal approach has its disadvantage of being a major surgery, which can cause nerve injuries precipitating constipation and mesh-related complications like, urinary incontinence, mesh erosion (7%-14%) and mesh infections/pelvic sepsis in 2%-16% of patients. [8, 9] The perineal approach can avoid these disadvantages and improve anal tone but has a higher recurrence rate over time and can cause de-novo bowel dysfunctions.
Few data in the literature is available which focuses on protocols for patient selection and treatment planned. The decision to choose the surgical approach is based on the anomalies involved. ODS is associated with rectocele and RI. [5, 10]; but unfortunately in spite of >100 procedures designed for this entity, none of the solo surgical procedures have maximum goal achievement in all fronts to date.
A fusion of current techniques or development of new techniques can help conform to goal optimization.
VMR also known as the Orr-Loygue procedure involves dissection of anterior as well as posterior rectum up to Levator-Ani muscle with meshes suturing from anterolateral rectal wall to sacrum. D’Hoore modified VMR involves dissecting only the Denonvillier’s fascia and mesh rectopexy (rectum fixed to sacral promontory via single mesh) recently done using the laparoscopic technique [11].
VMR is seen to have mitigated the complications commonly encountered in other methods of rectopexy like autonomic plexus damage is avoided as there is no need for dissection posterior to the rectum [12]. In a double-blind study by Hidaka J et al found that the gastrointestinal transit time is higher in the postoperative period in the laparoscopic posterior suture rectopexy (LPSR) method than laparoscopic VMR (LVMR). Also, the recurrence rate is significantly less with LVMR patients in long term follow-up; with improvement in functional outcome and reduced constipation [5,12].
LVMR has consistently shown lower recurrence rates (3%-4%), better pain scores, and overall complication rates when compared with Delorme’s(16%-38%) [5,13]. LVMR has longer operating time as compared with Delorme’s procedure but has acceptable short- and long-term outcomes. [7, 13] Additionally, the laparoscopic approach has shown prominent benefits in terms of reduced hospital stay, reduce pain scores and early return of bowel function; but has no significant difference between incidence of recurrence and morbidity [7].
In cases with complex rectocele and high-grade RI LVMR was extensively studied in a large series (n=264) by Laubert T et al where they found that overall the LVMR is a safe and effective technique for patients with ODS even in long-term follow-up (58.2 months) with 79.5% improvement in symptoms. They showed that there is 79.4% to 81.9% improvement in sigmoidocele and rectal prolapse (Grade II and III) respectively [8].
Mesh related complications are seen commonly in mesh rectopexy like infection and erosion and reports and studies with LVMR using biological meshes show early acceptable promising results with biological mesh. But due to a lack of long-term multi-centric RCT, it cannot be used routinely. If we close the peritoneal layer over the mesh theoretically mesh-related complications can be drastically minimized [9].
Chronically low internal and external sphincter pressures are noted in patients in ODS with anatomical anomalies like rectal prolapse, traumatic stretch related injury to the sphincters because of Rectal Intussusception and continuous stimulation of rectoanal complex reflex [7,14]. Many patients also have large rectocele because of weak perineum. These cannot be tackled by abdominal approach only and in our study, we found that a combined approach can correct these issues which may translate to improve the outcome
In one attempt to combine procedures to attend optimum results, the STARR procedure was combined with posterior rectal wall resection in patients with rectocele and rectal prolapse (Khubchandani’s procedure). STARR was looked upon as close to an ideal technique for ODS, but long-term (>3-12 months’ time) studies failed to keep up good ODS scores and hence the authors added the posterior rectal wall resection to improve ODS but it awaits long-term studies and RCT to prove its superiority [15].
In another study, TST (Tissue selecting therapy) STARR-Plus stapler device was used with larger resection volumes their series with RI and or rectocele. The authors showed a 6.7% recurrence rate at a median follow up of 23 months (range 12-30 months) and an overall improvement in symptoms. Cleveland Clinic Incontinence score did not show any statistical significance in preoperative and postoperative status. It also did not have well-defined scores for incontinence, constipation score and conservative treatments opted [16].
Long-term studies and multicenter data analysis lacks TST-STARR plus use in ODS, also there is a doubt that these score improvements are overestimated in many studies. Its use in ODS patients is still under scrutiny and newer standards to compare scores need to get developed [17,18].
It was seen by Madbouly et al that even though STARR showed acceptable outcomes in the immediate post-operative period the MODS and PAC-QOL scores declined after 18 months of follow-up [19].
In another RCT by Elshazly et al analyzed 66 patients with ODS and compared scores for STARR with modified Delorme’s procedure they found that scores are similar till one year of follow-up but it significantly improves in the later procedure [20].
It is important to note that the STARR procedure is not physiological as it involves full-thickness cutting of rectal muscle. This may lead to urgency and also cannot improve on the anal tone or strengthen the rectovaginal septum. Most of the studies demonstrate the equivalence of STARR and internal Delorme’s while some may suggest long term superiority of internal Delorme’s.
Being the safer of the two we have adopted the internal Delorme’s for the perineal procedure as the complication rates are very low and it increases the anal tone.
In a study by Gentile M et al sixty-six patients were evaluated with rectocele and RI or mucosal prolapse. Endorectal proctopexy with levatorplasty (ERPP) was compared with STARR. With an overall 12 months of follow-up, they found similar results and outcomes in both the groups. STARR was faster to perform but incurred higher cost and ERPP was more economical and patients had lesser dyspareunia [21].
Youseef M et al studied Delorme’s with levatorplasty, they found improved in continent patient (97.56% vs 70.73% P = 0.004), recurrence rate has statistically less in the latter group of patients (14.28% vs 2.43% respectively), mean anal pressure on the manometric study was seen much improvement in the latter group also the VAS satisfaction scores were better in the latter group (p=0.0001). Although the mean operating time was higher in the latter group the hospital stay was similar. This study shows that when Delorme is combined with levatorplasty it meets with the most satisfactory outcome. [14] Internal Delorme’s’ have a higher recurrence rate when done alone but reduces when done with levatorplasty (2.43%); rectal pressures, constipation are improved and lesser long-term morbidity.
A similar study aimed to combine anterior mucosectomy with posterior colpoperineorrhaphy was performed in 36 female patients with rectocele and anorectal prolapse. They found at 6-months of follow-up the need for self-digital maneuvering was not needed in any patients, 11% had persistent incomplete evacuation symptom. A statistically non-significant increase in dyspareunia (5.5% to 16%) was seen post-procedure [22].
LVMR is associated with less recurrence rate (3%-4%) that can be safely done to reduce RI, reduce or eliminate autonomic plexus damage due to avoidance of posterior rectal dissection and lesser short –term complications. [14, 23] If LVMR is done along with internal Delorme’s procedure as it will help reduce the recurrence, correct the high rectal or anorectal intussusception, augment and correct the pelvic floor strength and have improved long-term outcomes [7,10].
In this context, there are very few studies in the literature with small case series sharing their experience. We authors are of the opinion that a combination of transabdominal and transperineal approach is best suited for this group of patients with dual pathologies like a combination of intussusception, large rectocele, poor perineal body, poor anal tone and SRUS. In our opinion combining abdominal with a perineal approach in a selected group of patients may harness the benefits of both the procedures and will reduce the complications and recurrences. Our experience may open up new technical opportunities to tackle ODS due to RI and rectocele.
Conclusion
The combined approach can be used in a select group of people who have a combination of internal intussusception with rectocele, SRUS, poor perineal body, and a poor anal tone with prolapse. This may translate into better outcomes in patients.
Conflict of Interest: None