
Mohammad Rahimi1, Amirsaleh Abdollahi2, Amin Taheri Namaghi3, Amin Ghanbarpour Juybari 4* and Nazanin Reisi 5
1Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Mazandaran, Iran.
2Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Mazandaran, Iran.
3Doctor of Pharmacy Student, Student Research Committee, Pharmacy Group, School of Pharmacy, Mazandaran University of Medical Science, Sari, Iran.
4Anesthesiologist Mazandaran University of Medical Science, Sari, Iran Iran.
5Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran.
*Corresponding author: Amin Ghanbarpour Juybari, Anesthesiologist Mazandaran University of Medical Science, Sari, Iran Iran.
Received Date: June 17, 2024
Accepted Date: July 01, 2024
Published Date: July 05, 2024
Citation: Mohammad Rahimi, Amirsaleh Abdollahi, Amin Taheri Namaghi, Amin Ghanbarpour Juybari and Nazanin Reisi. (2024) “Comprehensive Management of Acne Vulgaris: Integrating Non-Antibiotic Therapies to Mitigate Resistance and Drug-Induced Discomfort and Pain Management.” Case Reports International Journal, 2(1); DOI: 10.61148/CRIJ/004.
Copyright: © 2024 Amin Ghanbarpour Juybari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Acne vulgaris management requires a multifaceted approach considering genetic predispositions, lifestyle factors, and skincare practices. Topical agents like isotretinoin, benzoyl peroxide, salicylic acid, and adapalene remain pivotal, but antibacterial resistance presents a growing concern. Clindamycin and erythromycin, once mainstays, face challenges due to resistance, advocating for combined therapy and limiting monotherapy duration. Guidelines recommend doxycycline and minocycline over tetracycline and azithromycin, coupled with benzoyl peroxide or retinoids. Non-antibiotic approaches like comedone extraction, cryotherapy, chemical peels, and optical treatments offer promising avenues for treatment-resistant acne. Addressing resistance, prudent antibiotic use is crucial, advocating for combined therapy and limiting monotherapy duration. Benzoyl peroxide emerges as pivotal due to its lack of specific resistance. Isotretinoin, salicylic acid, azelaic acid, sulfur, and alpha-hydroxy acids provide alternative treatments, with oral contraceptive pills and spironolactone offering hormonal acne management. Emerging agents like clascoterone provide novel avenues. Tailored, evidence-based strategies are essential for managing acne while mitigating antibacterial resistance
skincare practices
Introduction:
acne vulgaris is a common and often persistent skin condition that affects a significant portion of the population. Understanding the multifactorial nature of acne development, including genetic predisposition, nutrition, lifestyle factors, and skincare practices, is crucial for effective management. By employing a comprehensive approach that considers individual characteristics and tailors treatment options accordingly, dermatologists can help alleviate the burden of acne and improve the quality of life for those affected by this condition.
When it comes to treatment options, various topical agents such as isotretinoin, benzoyl peroxide, salicylic acid, and adapalene, among others, can be effective in managing acne lesions. Oral contraceptives, spironolactone, and clascoterone have shown promise in hormonal acne management. Additionally, procedures like comedone extraction, cryotherapy, chemical peels, and optical treatments can be employed for acne that does not respond well to conventional treatments.
The management of acne involves targeting factors such as sebaceous hypersecretion, abnormal keratinization, colonization of C. acnes bacteria, and the inflammatory process. Treatment options depend on the type and severity of acne.
Topical therapy, including retinoids (adapalene and tretinoin), antimicrobials like benzoyl peroxide, and antibiotics, is commonly used for mild to moderate acne. Other topical medications like azelaic acid, salicylic acid, nicotinamide, sulfur, zinc, and alpha-hydroxy acids can also be effective in treating acne.
To prevent antibacterial resistance, the simultaneous use of multiple antibiotics is recommended, along with the inclusion of benzoyl peroxide to reduce the risk of resistance. Tetracycline and azithromycin should be used cautiously due to the increased risk of antibiotic resistance.
Isotretinoin (Roaccuatne®) is considered the most effective and potent treatment for severe acne that does not respond to other therapies. It significantly reduces sebum secretion, comedone formation, bacterial load, and inflammation. However, isotretinoin has potential side effects, including teratogenicity, dryness of the skin and mucous membranes, and laboratory abnormalities. Proper skin care, including gentle cleansing, barrier repair, and sun protection, is essential during isotretinoin treatment.
Overall, a comprehensive approach that combines different treatment modalities, considering the individual's characteristics and the type of acne, is crucial for achieving successful outcomes in acne management. Regular follow-up and adherence to treatment protocols are essential for optimal results.
How to prevent antibacterial resistance
Clindamycin 1% and erythromycin 2% are topical antibiotics that are used in the treatment of acne. Observing the occurrence of resistance in some acne when using erythromycin has made the use of clindamycin a priority over erythromycin(1)
The simultaneous and combined use of drugs and antibiotics is recommended due to the reduction of antibiotic resistance. The use of monotherapy is not recommended due to the increased risk of antibiotic resistance(1)
Clindamycin and erythromycin are two antibiotics primarily used in the past to treat acne. Due to frequent use in the past and familiarity of acne with the mechanism of action of these drugs and resistance to them, currently, they cannot be classified as the most effective drugs in the treatment of acne(2)
The possibility of antibiotic resistance in the treatment of acne when we use only one antibiotic is much higher than when several antibiotics are used at the same time; for this reason, the use of monotherapy in the treatment of acne is not recommended, or it is only safe for 3 months. After 3 months, combined treatment with other drugs, such as benzoyl peroxide (BPO), which has a lower risk of resistance, should be put on the agenda. It is better to avoid combined treatment of topical and oral antibiotics together(2)
According to AAD (American Academy of Dermatology) studies, doxycycline and minocycline are more effective than tetracycline and azithromycin, and their use in the treatment of acne is preferable as the primary drug. Simultaneous use of tetracycline and macrolides(Azithromycin, clarithromycin, and erythromycin) increases the risk of antibiotic resistance and is not recommended(1)
According to the guidelines for treating acne, systemic antibiotics such as doxycycline and minocycline are recommended for treating moderate-severe acne over 3-4 months. According to the guidelines, it is better to use BPO or retinoids together with topical antibiotics to reduce the risk of antibiotic resistance. In the treatment of acne, the use of doxycycline antibiotic is a priority. The use of monotherapy is not recommended. Recently, SPAUD (The Scientific Panel on Antibiotic Use in Dermatology) has reported several recommendations for better effectiveness of antibiotic treatment against acne. 1. Avoiding indiscriminate use of topical antibiotics and using them in cases where clinical evidence is observed 2. Simultaneous use of BPO to prevent drug resistance 3. Avoiding monotherapy in the treatment of acne 4. Avoiding using more than the limit of oral antibiotics (preferably to be used in a period of 3-4 months together with BPO and retinoids) 5. we can use other methods for treatment and not limit ourselves only to antibiotic treatment(3)
Benzoyl peroxide( BPO) is one of the most famous and common drugs in the treatment of acne(4) The reason should be stated that no specific drug resistance against BPO has been found, and for this reason, its use is widespread(2)
BPO can be used both as monotherapy within 1-2 months (since specific resistance against it has not been proven) and as combined treatment with antibiotics and other retinoids (due to the risk of antibiotic resistance reduced)(1, 2)
Concomitant use of topical antibiotics with BPO or retinoids in the treatment of acne has been shown to be a perfect way to reduce the risk of antibiotic resistance(5) BPO, like any other drug, leaves a series of side effects such as burning, dryness, erythema, stinging & peeling(2)
According to recent studies, it has been proven that combined treatment of clindamycin with BPO or retinoids has two important advantages, including 1. elimination and treatment of acne 2. antibiotic resistance against erythromycin and clindamycin is reduced(5)
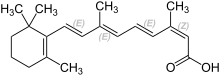
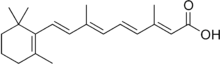
Isotretinoin is one of the best, most effective, and most potent drugs to treat acne(4). Isotretinoin is from the vitamin A family(1). This drug is used to treat very severe or antibiotic-resistant Acne or Acne that makes a person mentally and socially depressed.(1, 4) Isotretinoin is the only effective drug in the world that affects all four factors of acne production(1.Excess oil (sebum) production.2.Hair follicles clogged by oil and dead skin cells.3.Bacteria.4.Inflammation)(2) The mechanism of action of this drug is on the sebaceous glands of a person suffering from acne. Through processes, it leads to the reduction of sebum and fat production from these glands.(3)
The duration of treatment with this drug is 4-6 months, and after this period, unique results of the treatment will be seen(2) The dosage of this drug depends on the stage of treatment at the time of drug use, but to start the treatment, 0.25-0.4 mg/kg per day is recommended(1) Like any other drug, isotretinoin has its side effects, such as musculoskeletal problems, dry skin, weight loss, and mild side effects related to vision(3)
Triclosan is one of the antibacterial drugs against which specific antibiotic resistance has not been found and is effective.(2)
During the treatment, when we did not respond effectively to local antibiotic treatment, we tried to replace it with oral systemic antibiotics.(2)
In treating moderate to severe acne, oral antibiotics should be used, and in the use of oral antibiotics, doxycycline and minocycline (Minocin) are preferred over tetracycline. Also, simultaneous use of BPO along with oral antibiotics is highly recommended to prevent resistance to oral antibiotics.(4)
Among the two drugs, tetracycline and azithromycin, the use of tetracycline is better because of the risk of antibiotic resistance.(4)
Isotretinoin (Roaccuatne®) :
Since its 1982 introduction, isotretinoin has been used to treat severe acne with nodular and cystic formations as well as resistant acne that does not respond to other treatment modalities. It is the most effective drug for treating acne. A first-generation retinoid approved for treating severe acne vulgaris is oral isotretinoin (13cis-1retinic acid), a synthetic analog of vitamin A. Only when topical therapy and appropriate response to systemic antibiotics like doxycycline cannot be achieved within a three-month course of therapy can isotretinoin be used as a second-line treatment for acne. Practically, isotretinoin has benefits for mild to moderate acne and a variety of "off-label" uses, in addition to severe forms of acne(6, 7).
Although acne is primarily an adolescent disorder (12 years old until 18), it can also affect adults(8).
According to European recommendations, isotretinoin should be taken daily for at least six months at a dose of 0.3 to 0.5 mg/ kg. The length of the treatment period may be extended if there is insufficient response. Relapsed cases, or acne retrial, may need two or three courses of isotretinoin(9).
Patients with acne experience an improvement in their quality of life as a result of using isotretinoin. Isotretinoin has some side effects and complications, such as teratogenicity, liver dysfunction, and mood disorders like depression, in addition to its outstanding anti-acne effect, making it the first treatment choice for severe acne(10, 11).
Mechanism of Action:
Isotretinoin is the most effective treatment for acne because it reduces sebum secretion, comedone formation, and bacterial load and anti-inflammatory effect.(10, 11).
Side Effects:
There are adverse effects of isotretinoin. With the exception of teratogenicity, the majority are dose-related. Isotretinoin has fewer non-serious side effects than oral antibiotics plus topical agents. Isotretinoin's most common side effects are skin-related and linked to xerosis. Additionally, during isotretinoin therapy, dry nasal membrane has been observed in 2/ 3 of patients, which can cause epistaxis. Nasal complications are generally not life-threatening, particularly when taking low-dose isotretinoin(8, 9).
Isotretinoin treatment disturbs nasal mucociliary clearance significantly, which reduces normal and regenerated mucosal thickness, causing severe inflammation, increasing the reactive changes in the respiratory epithelium, and higher recruitment of neutrophils in the nasal surface mucosa. Nasal moisturizers (d‐panthenol, vaseline, glycerin, hypertonic solutions, and hyaluronic acid) are also recommended for these patients(12).
Side effects may be categorized as:
1) teratogenic
2) clinical: cutaneous or extracutaneous
3) laboratory findings(13, 14).
Oral isotretinoin treatment has had the greatest therapeutic impact on acne, improving symptoms markedly. Acne has a substantial psychological impact, manifesting mainly as depressive symptoms. Most studies have found a beneficial effect of reduced depression symptoms with the treatment(15).
Teratogenicity:
Ingestion of oral isotretinoin in female patients of childbearing potential, independently of the dose, may induce major fetal malformations, premature birth, or spontaneous abortion in a high percentage of cases. This is the most critical side effect(16, 17).
Cutaneous Side Effects:
The most common clinical side effect is cheilitis, a dryness of the lips that may range from simple xerosis to painful fissures. Dry skin and desquamation are frequently experienced in a dose-dependent manner where sebaceous glands are most prevalent, namely the face, chest, and back(18, 19).
Extracutaneous Side Effects:
During treatment, patients may experience headaches, fatigue, eye conditions like keratitis and corneal opacities, and visual disturbances at night. These conditions can occasionally be drug-related and dose-related. When isotretinoin and specific antibiotics are combined, benign intracranial hypertension has been documented. When taking isotretinoin, gastrointestinal disorders linked to colitis and inflammatory bowel disease may develop(20).
Laboratory Abnormalities:
Lipids: Blood cholesterol and triglyceride levels may rise due to oral isotretinoin use. Before beginning treatment, six weeks later, and then every three months thereafter, cholesterol and triglyceride levels are checked. Oral isotretinoin should be stopped if hypertriglyceridemia cannot be controlled(21).
Liver transaminases: While receiving treatment, liver transaminases may also rise, with a dose-dependent effect. Unless more frequent monitoring is clinically necessary, transaminases should be checked before treatment, six weeks later, and then three times per month after that(22).
Creatinine phosphokinase (CPK): Exercise increases the physiological activity of the muscle enzyme creatinine phosphokinase(CPK). It is well known that moderate physical activity, which many teenagers engage in, raises CPK levels. Another potential inducer has been thought to be oral isotretinoin(23).
Summary of side effects:
A successful way to achieve good clinical results while minimizing side effects compared to a standard dose of 0.5 mg/ kg/ day (57, 72) is to start daily doses of 0.01 to 0.02 mg, or roughly 10 mg per day, and gradually increase to the highest dose tolerated by the patient. The most effective medication for treating severe acne that does not respond to other treatments is oral isotretinoin, without a doubt. Without stating that the only real issue is teratogenicity in female patients of childbearing age, for which risk management plans are in place, as described above (48), it is occasionally incorrectly described in broad brush strokes as a dangerous drug(19, 24).
Proper skin care while receiving isotretinoin treatment:
Gentle cleansing, cutaneous barrier repair, and barrier function maintenance are necessary for appropriate skin care for acne vulgaris treated with retinoids. Use gentle soaps, micellar cleansing lotions, or cleansing emulsions when cleaning. Avoid using abrasive cleaners containing sulfur, glycolic acid, or another similar substance. Hydrolyzed and emollient products should have an aqueous base, non-comedogenic, hypoallergenic, non-irritating, and not greasy. Utilizing moisturizers with active ingredients of a high enough quality and concentration to protect and heal the skin is crucial. It is appropriate to use products containing hyaluronic acid, glycerin, biosaccharides, or similar substances(25-27).
Dermatitis, eczema, cheilitis, and other symptoms of solar sensitivity are common in photo-exposed areas, particularly on the face, hands, and arms, during times of high solar exposure, and particularly in nations with thinning ozone layers. When exposed to the sun, reapplied every two hours, and after swimming or perspiring, use an SPF 50+ UVA/ UVB solar protector that has been tested explicitly for comedogenicity in oily, acne-prone skin. Petroleum jelly at night and lip balms with an SPF 30– 50 filter applied several times per day are advised for the lips and mucous membranes. Patients who wear contact lenses or reside in areas with high air pollution levels can benefit, especially from eye drops and gels. Particularly in the summer and when participating in any outdoor activities, sunglasses should be worn(26, 28).
Benzoyl peroxide:
A peroxide family organic substance used to treat acne. As a peeling agent, it functions. In addition to acting as a direct antimicrobial agent, it promotes skin turnover, clears pores, and lowers the number of bacteria. When used in conjunction with other acne vulgaris treatments, benzoyl peroxide has mild sebostatic and keratolytic effects. Drug resistance has not seemed to develop with benzoyl peroxide use, in contrast to other topical antibiotics. In many nations, including those in Europe and the USA, where the corresponding medical guidelines recommend it as the standard treatment for acne vulgaris, topical benzoyl peroxide has been used to treat the condition(29-31).
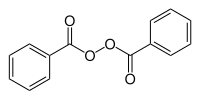
Compared to Cutibacterium acnes, a crucial component of acne vulgaris, topical benzoyl peroxide has bactericidal effects. After being absorbed by the skin, benzoic acid is produced from benzoyl peroxide. The renal system systemically absorbs and excretes about 5% of benzoic acid. Cyanine in the skin breaks down the remaining benzoic acid, releasing active free-radio oxygen species that oxidize bacterial proteins. Lipids, free fatty acids, and P. acnes are all reduced in order to improve acne vulgaris(30, 32, 33).
Similar to results obtained after four weeks of antibiotic therapy, 10% benzoyl peroxide applied daily for two weeks reduced the number of P. acnes in hair follicles by 98% and the free fatty acids by 50%. The mild sebostatic effects of topical benzoyl peroxide also help to treat comedonal acne and increase keratolytic activity. By stimulating the healthy production of granulation tissue and the quick ingrowth of epithelium, benzoyl peroxide successfully treats cutaneous ulcers(30, 33, 34).
The bleaching property of benzoyl peroxide is its most frequent drawback, possibly resulting in the discoloration of colored fabrics and hair whitening. Topical benzoyl peroxide causes scaling, erythema, and mild dryness at higher concentrations. Patients who exhibit pronounced erythema and irritation at the treatment site should be suspicious because there have also been case reports of contact dermatitis in a small percentage of patients. The best course of action in these situations is to stop using benzoyl peroxide. To reduce the risk of phototoxicity and skin irritation, patients should limit their UV exposure and wear sunscreen(35).
Topical sulfone products, such as dapsone, should not be used in conjunction with topical benzoyl peroxide because it is said to cause skin and facial hair to turn yellow. Topical hydroquinone and topical benzoyl peroxide should not be used concurrently because they may cause more skin irritation and temporary epidermis staining. It has been documented that topical benzoyl peroxide and oral isotretinoin use together causes dryness and increased skin irritation(36-38).
Topical benzoyl peroxide and topical tretinoin should not be administered simultaneously because doing so reduces the drug's effectiveness. Adapalene is a suitable combination product and is resistant to benzoyl peroxide oxidation, unlike tretinoin. Topical anesthetic efficacy is reportedly reduced when topical benzoyl peroxide is used in conjunction with topicals. The treatment area should be thoroughly cleaned before topical anesthetic application for best results(32, 39).
Salicylic Acid:
For more than 2,000 years, various skin conditions have been treated with salicylic acid. Salicylic acid is a helpful peeling agent because it can exfoliate the stratum corneum. Salicylic acid is a useful peeling agent for acne patients in particular because of its comedolytic properties. Salicylic acid once thought of as a keratolytic agent, is now recognized and discussed in this article because of its ability to disrupt cellular junctions rather than sever or lyse intercellular Keratin filaments(40).
Salicylic acid is 2 hydroxybenzoic acid, also known as orthohydrobenzal acid chemically. Willow bark, sweet birch, and wintergreen leaves are sources of salicylic acid and salicylates. However, salicylic acid can also be synthesized artificially(41, 42).
In contrast to hydroxy acids (such as glycolic acid), salicylic acid is lipid-soluble, making it miscible with the sebaceous gland and epidermal fatty acids in hair follicles. Although the precise mechanisms at work are unknown(42), salicylic acid has keratolytic and comedolytic properties. Additionally, salicylic acid lessens sebum secretion in acne patients, which increases its therapeutic value in these patients(43). Corneocyte adhesion is reduced by salicylic acid (44), which also loosens these cells and leads to their subsequent detachment. Intercellular lipids, which are covalently linked to the cornified envelope enclosing the surface epithelial cells, are removed by salicylic acid, a lipophilic agent. In chemical skin peeling, many dermatologists have used salicylic acid's antihyperplastic effect on the epidermis (45, 46).
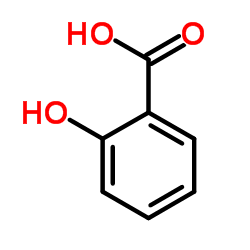
Desmosomes, made up of various proteins, including desmoglein, are necessary for the skin's epidermal cells to adhere. Desmosomal proteins, including desmogleins, are extracted by salicylic acid, an organic acid, it has been discovered. Exfoliation results from the loss of epidermal cell cohesion due to this action. Because salicylic acid works by disrupting cellular junctions rather than breaking or lysing intercellular keratin filaments, it should now be considered a desmolytic agent compared with a keratolytic one in terms of its mechanism of action(47, 48).
Although the literature on dealing with salicylic acid is well-documented, there are some unfavorable side effects (Prolonged erythema, Intense exfoliation, Crusting, Dryness, Pigmentary dyschromia, Systemic toxicity(salicylism), Hypoglycemia, Contact sensitization) that are typically mild and fleeting. Topical moisturizers can be applied frequently to control dryness, crusting, and hyperpigmentation. No cases of scarring or lingering post-inflammatory dyschromia were reported(40).
Adapalene:
Essential topical agents for treating acne are nutritional retinoids, also referred to as vitamin A derivatives. Tretinoin, tazarotene, and adapalene are the three active substances used in these. Each of the three retinoids exhibits slight variations in efficacy and tolerability due to binding to various sets of receptors. They reveal their anti-comedogenic, anti-inflammatory, and immunomodulatory effects by modulating human keratinocyte gene expression and transactivation. However, the use of topical retinoids is constrained by cutaneous side effects like irritation, erythema, dryness, and peeling. Adapalene is the least irritating substance of the three retinoids mentioned above. 14 Tretinoin was combined with the topical antibiotic clindamycin as a fixed combination reducing the irritation potential and increasing therapeutic efficacy(49, 50).
A third-generation retinoid with anti-inflammatory, comedolytic, and anti-comedogenic properties is called adapalene. By reversing the abnormal follicular keratinization process and preventing the formation of microcomedon, it lowers the number of inflammatory lesions and comedones. Compared to other retinoids, this agent is better tolerated and has a lower risk of causing cutaneous side effects(50, 51).
Tazarotene:
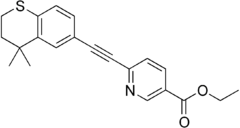
A new generation of receptor-selective synthetic retinoids called tazarotene (TZR) 6-] 2- 4, 4' dimethylthiochroman's ethyl) nicotinic acid ester is used for acne vulgaris. According to studies on dermal safety, TZR lacked phototoxic or photoallergic potential1– 3. However, a sizable portion of users may experience adverse side effects like pruritus, burning or stinging, and erythema during treatment, typically prolonged (weeks or months)(52-54).
Tretinoin:
To treat mild to moderate acne, tretinoin (all-trans retinoic acid) has historically been used as a comedolytic agent. It has been demonstrated that it can encourage the development of new cells, clear pores, and encourage normal sebum flow. Since the host benefits from removing harmful bacteria, their extracellular byproducts, and other pro-inflammatory debris, homeostatic phagocytosis may be regarded as an anti-inflammatory response. Tretinoin's comedolytic-related activity has long been understood(55).
Tretinoin's comedolytic-related activity has long been understood. Tretinoin normalizes the exfoliation of the pilosebaceous unit's follicular epithelium, inhibits transglutaminase activity, prevents follicular plugging, drains and expels excess sebum and P. acnes, and contributes to the development of an aerobic environment that less prone to these conditions(56-58).
Nearly 50 years ago, tretinoin was first used as a topical anti-acne agent. Understanding the potent comedolytic-related properties and developing an appreciation of its anti-inflammatory properties have led to positive effects of beneficial effects. Tretinoin has five significant comedolytic-related properties that can be regarded as an anti-inflammatory in nature, as well as 17 other potential activities that may help to control the inflammatory cascade of acne and the production of associated inflammatory vectors, according to a thorough review of its immunomodulating properties(59).
Phagocytic function, respiratory burst, inducible nitrous oxide synthase (iNOS) activity, degranulation, and proteolytic enzyme activity are the five distinct inflammatory events linked to acne and phagocytosis. According to the available data, tretinoin effectively modulates each of them(55).
Topical tretinoin is incredibly safe. Because only 1% of the drug applied to the face is absorbed and the amount that does reach the circulation does not change plasma vitamin A levels, there are essentially no systemic side effects(60).
Tretinoin has recently been used in topical combination treatments for acne along with antibacterial like erythromycin, benzoyl peroxide, and clindamycin. The topical use of clindamycin and tretinoin as a combination treatment modality with antibacterial, comedolytic, and anti-inflammatory properties has been shown to be a very effective therapy for treating the various stages of acne. Up to 14 potential activities were discovered that could have immunomodulating effects(55, 61, 62).
Azelaic acid:
Azelaic acid is known as a naturally establishing saturated dicarboxylic acid that has been demonstrated to work at treating acne when used topically (typically as 20% cream). Twice daily topical application of 20% azelaic acid cream was markedly more effective than that of its vehicle in reducing the numbers of comedones, papules, and pustules in patients with mild-to-moderate acne. The cream was of comparable efficacy to topical 0.05% tretinoin cream, topical 5% benzoyl peroxide gel, topical 2% erythromycin cream, and oral tetracycline 0.5 to 1.0 g/day. Topical 20% azelaic acid was significantly less effective in treating conglobate acne than oral isotretinoin, which was given twice daily for six months(63).
Azelaic acid may pass as an anti-acne drug by inhibiting the Propionibacterium acne (P. acne) thioredoxin reductase enzyme, which prevents the cytoplasmic activity of bacterial GENETICS. Azelaic acid has to pass through L. acnes' thick peptidoglycan in order to enter the assize corneum, sebaceous tissues, and cytoplasm(64, 65).
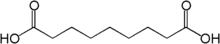
Azelaic acid has demonstrated no systemic adverse effects. Local cutaneous irritation, marked by erythema, pruritus, scaling, and a burning sensation, occurs in 5 to 10% of patients (an incidence comparable to that seen with its cream base), and is mild and transient, generally subsiding after 2 to 4 weeks of treatment(63).
Sulfur:
Antifungal, antibacterial, and keratolytic properties exist in sulfur. Sulfur applied topically rarely causes negative effects. It absolutely was commonly used in the last to take care of dermatological disorders like acne vulgaris(66).
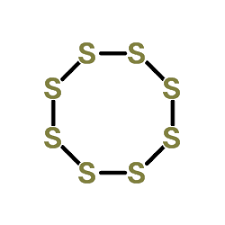
Sulfur that has been applied topically absorbs systemically about 1%. Sulfur applied topically rarely causes adverse effects, which are mainly skin-specific(67).
Sulfur is effective for treating several dermatological conditions and can cause histological changes when applied topically, such as hyperkeratosis, ecstasy, and dilatation of the skin vasculature. Sulfur was found to be comedogenic when used on human and rabbit skin during one study, a finding that various other studies did certainly not confirm(67).
Alpha‐hydroxy acids:
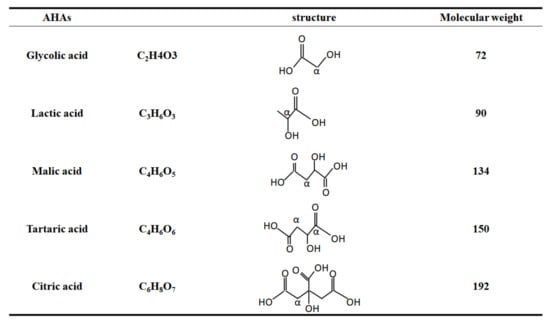
Organic acids, known as AHAs, have a single hydroxyl group attached to their alpha position. Many AHAs are commonly used in cosmetic products, such as glycolic, lactic, malic, tartaric, and citric acids. In dermatology, AHAs have also been used to improve the appearance of acne pimples, keratoses, and superficial peeling agents. When using AHA-containing products, patients must be cautious because some side effects, such as swelling, burning, and pruritus, may occur(68).
It has recently been acknowledged that home cures and hydroxy acid (AHA) peels are crucial adjunctive therapies for acne. AHAs have recently been proven to improve these disorders by thinning the stratum corneum, encouraging epidermolysis, dispersing basal layer melanin, and improving dermis collagen synthesis. However, their precise mechanism of action is unknown(69).
Oral Contraceptive Pills(OCP):
Medical professionals have long recognized oral contraceptive pills (OCPs) as having the ability to reduce the incidence of acne and the number of acne lesions. The mechanism by which OCPs treat acne most likely involves lessening androgen levels in the blood. Especially, OCs increase the production of sex hormone-binding globulin, while decreasing total and bioavailable testosterone. Additionally, pituitary gonadotropin secretion is suppressed by the steroids in OCPs, which lowers ovarian androgen levels(70, 71).
Vomiting, bloating, and breast tenderness are just some side effects(72)(72)(72)(72)(72)(72)(72)(72)(72)(72)(72)(72)(72)(72)(128)
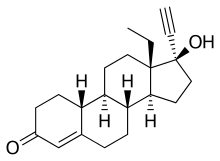
Levonorgestrel
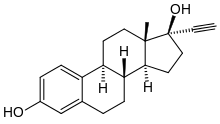
Ethinylestradiol
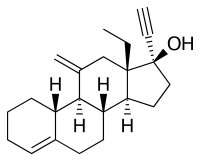
Desogestrel
However, over the past 30 years, more and more people have started using combined estradiol-progestin oral contraceptive pills (OCPs) to manage their acne, appreciating it to the added advantage of lowering the risk of unintended pregnancy. OCPs have a very different mechanism of action from antibiotics, which could be seen as more preventive than helpful. The estrogen component, which decreases ductal plugging and sebum production to stop the development of new acne lesions by reducing the amount of free androgens in the body, is primarily responsible for their effectiveness. More recently, the progestin components reduce androgenicity and antiandrogetic activity has decreased OCPs' ability to cause acne(73, 74).
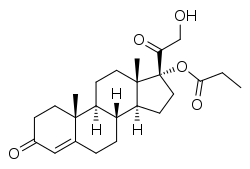
Spironolactone:
A non-selective mineralocorticoid receptor antagonist with a moderate affinity for both progesterone and androgen receptors is the synthetic 17-lactone steroid spironolactone. Although spironolactone has been used off-label for acne since the 1980s, it is primarily used in the medical process as a potassium-sparing diuretic. By inhibiting androgen-induced sebocyte proliferation and blocking dihydrotestosterone's ability to bind to the androgen receptor in sebocytes, it is possible to reduce the amount of sebum(75).
Although it may be unlikely at therapeutic doses, spironolactone's systemic effects on the synthesis of androgen precursors by the adrenal gland may also help with clinical efficacy. Women who experience premenstrual acne flares associated with fluid retention may benefit from spironolactone's diuretic effects(76).
Women's irregular menstruation, urinary frequency, headaches, nausea, vomiting, breast tenderness, and breast enlargement are common side effects of long-term use of spironolactone for acne treatment(77).
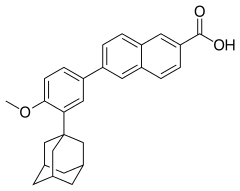
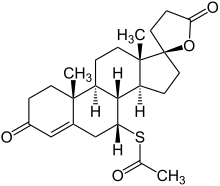
Clascoterone:
clascoterone is a 17-alpha-propionate (17a, 21-hydroxy-4-pregnene-3, 20-dione-propione) dihydroxylone. Its molecular formula is C24H34O5.18, and because it shares a fused four-ring backbone with DHT, it is structurally similar to that substance(78, 79).
The topical activity of closcoterone is selective. It has been discovered to have a strong in vitro affinity for the androgen receptor. It limits the binding of androgen receptors and competes with them, particularly DHT, which prevents downstream signaling of acne pathogenesis-related pathways. In human primary sebocytes, it inhibits androgen-receptor-regulated gene transcription and dose-dependently antagonizes lipid and inflammatory cytokine production. With the exception of a weak glucocorticoid activity, cortexolone, an intermediate in the biosynthesis of glucocorticoid, does not have an endocrine function. According to studies done on reconstructed epidermis, Clascoterone does not affect 5-alpha reductase and does not prevent testosterone from being converted to 5HT(79-81).
Dermal papilla cells are negatively impacted by dihydrotestosterone's (DHT) effects, which are the antagonist of clascoterone. Additionally, it reduces sebum secretion, hair miniaturization, and dermal inflammation while reducing prostaglandin D2 and interleukin 6 production(82).
1% (10 mg/ g) cream of closcoterone is available. It is recommended that patients twice daily apply a thin layer to the damaged region(83).
Topical clascoterone has mild, rare, and primarily localized skin reactions side effects. Application site dryness, scaling, erythema, hypertrichosis, pain, contact dermatitis, hair color changes, eye irritation, peritonsillar abscess; dysgeusia; headache; oropharyngeal pain; and application site hypersensitivity are some of the side effects that have been reported. Some study subjects have been found to have elevated potassium levels. According to long-term safety studies, male participants have not experienced systemic antiandrogenic effects like decreased libido or feminization(78, 79, 84, 85).
Resorcinol:
a substance found in many acne treatment products that contain dihydroxybenzene. By removing the accumulation of dead skin cells, it aids in the prevention of comedones(29).
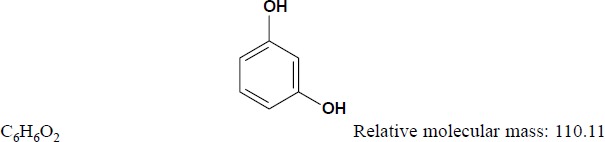
Due to thyroid effects, resorcinol is thought to be an endocrine disruptor. It may also affect iodine uptake and appear to inhibit thyroxin peroxidase. When used dermally to treat skin ulcers, resorcinol has resulted in hypothyroidism. Resorcinol also irritates the eyes and skin, and although it appears that cases of skin sensitization in humans are uncommon, it may cause skin contact. According to pharmacokinetic studies, resorcinol is quickly metabolized and absorbed through oral, dermal, and subcutaneous routes. Urine excretion mostly takes the form of conjugates of glucuronide and sulfur. Although there is little information available on the kinetics of resorcinol excretion in humans, rat data indicates that it excretes quickly and that more than 80% of orally-administered radioactive material is eliminated through urine within the first 24 hours(86).
Resorcinol and sulfur are commonly found together in acne products. Resorcinol helps prevent comedons by eliminating the accumulation of dead skin cells(87).
Anesthetic consideration:
Some individuals may experience pain or discomfort after using certain anti-acne medications, particularly those that are applied topically or taken orally. Understanding and managing this pain is essential to ensure patient compliance and overall treatment success.(88)
Topical medications, such as retinoids (e.g., tretinoin, adapalene) and benzoyl peroxide, are common treatments for acne vulgaris. While these medications are generally well-tolerated, they can cause skin irritation, dryness, and peeling, especially during the initial stages of treatment. This irritation may manifest as a burning or stinging sensation, particularly in individuals with sensitive skin or those using higher concentrations of the medication.(89)To alleviate pain and discomfort associated with topical acne medications, dermatologists may recommend several strategies. First, patients should be advised to start with lower concentrations of the medication and gradually increase the strength as tolerated. Additionally, applying a moisturizer or emollient cream before or after applying the medication can help hydrate the skin and reduce irritation. Patients should also be instructed to avoid harsh or abrasive skincare products that may exacerbate irritation.(90)Oral medications, such as oral isotretinoin (Accutane), may also cause pain or discomfort as a side effect. Common side effects of oral isotretinoin include dryness of the lips, nose, and eyes, as well as musculoskeletal discomfort and headaches. Patients experiencing these side effects should be encouraged to stay hydrated, use lip balm and moisturizing eye drops, and practice gentle skincare to alleviate dryness and discomfort.In some cases, individuals may experience gastrointestinal symptoms such as abdominal pain, nausea, or diarrhea while taking oral acne medications. These symptoms can be distressing and may affect treatment adherence. (91, 92)Patients should be advised to take oral medications with food to minimize gastrointestinal upset and consider dividing the dose throughout the day if necessary. Managing pain associated with acne vulgaris and its treatment involves a comprehensive approach aimed at minimizing discomfort and optimizing treatment outcomes. Here are several strategies for pain management in the context of acne treatment: Topical Anesthetics: Dermatologists may recommend the use of topical anesthetics to numb the skin and reduce pain associated with acne lesions or treatment procedures. These topical agents, such as lidocaine or benzocaine, can be applied directly to the affected area before applying acne medications or undergoing procedures like comedone extraction or chemical peels.(93)Cold Compress: Applying a cold compress or ice pack to the skin can help numb the area and reduce pain and inflammation associated with acne lesions or irritated skin. Patients can gently apply a cold compress to affected areas for short periods to alleviate discomfort.(94)Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs, such as ibuprofen or naproxen, can help alleviate pain and inflammation associated with acne lesions or side effects of acne medications. These medications can be taken orally as directed by a healthcare provider to provide temporary relief from discomfort.(95)
Topical Moisturizers: Using gentle, non-comedogenic moisturizers can help soothe and hydrate the skin, reducing irritation and discomfort associated with topical acne medications. Moisturizers containing ingredients like ceramides, hyaluronic acid, or colloidal oatmeal can help restore the skin barrier and alleviate dryness and itching.(96)Pain-relieving Creams or Gels: Certain over-the-counter creams or gels containing ingredients like menthol, camphor, or capsaicin can provide temporary relief from pain and itching associated with acne lesions. These products can be applied topically to the affected area as needed to alleviate discomfort.(97)Stress Management Techniques: Stress can exacerbate pain and inflammation associated with acne vulgaris. Encouraging patients to practice stress-reduction techniques such as deep breathing, meditation, yoga, or progressive muscle relaxation can help minimize pain and improve overall well-being.(98)Gentle Skincare: Using mild, non-irritating skincare products can help prevent further irritation and discomfort associated with acne treatment. Patients should be advised to avoid harsh cleansers, abrasive scrubs, and excessive rubbing or scrubbing of the skin, which can exacerbate pain and inflammation.(99)Adjusting Treatment Regimens: If pain or discomfort persists despite the use of pain management strategies, dermatologists may consider adjusting the patient's treatment regimen. This may involve switching to alternative acne medications, adjusting medication strengths or dosages, or incorporating additional pain management techniques.(100)
conclusion:
In conclusion, Benzoyl peroxide is an effective treatment for acne vulgaris due to its antimicrobial and exfoliating properties. It reduces bacteria, clears pores, and promotes skin turnover. It is well-tolerated, although it may cause bleaching of fabrics and mild skin irritation.
Salicylic acid is a peeling agent that disrupts cellular junctions and exfoliates the skin. It is effective in treating acne and has minimal side effects such as mild and transient skin irritation.
Adapalene is a retinoid with anti-inflammatory, comedolytic, and anti-comedogenic properties. It reduces the formation of inflammatory lesions and comedones and is well-tolerated compared to other retinoids.
Tazarotene is a synthetic retinoid used for acne vulgaris. It may cause prolonged side effects such as pruritus, burning, and erythema.
Tretinoin is a vitamin A derivative that acts as a comedolytic agent. It promotes cell turnover, clears pores, and has anti-inflammatory effects. It is generally safe for topical use.
Azelaic acid is effective in treating acne and reduces the number of comedones, papules, and pustules. It is well-tolerated with minimal side effects.
Sulfur has antifungal, antibacterial, and keratolytic properties. It is generally safe and rarely causes adverse effects.
Alpha-hydroxy acids (AHAs) are used as peeling agents and can improve the appearance of acne. They may cause mild side effects such as swelling and pruritus.
Oral contraceptive pills (OCPs) can reduce acne by decreasing androgen levels. They are commonly used for both acne treatment and contraception.
Spironolactone is a diuretic with antiandrogen properties. It reduces sebum production and is often used in women with hormonal acne. Side effects may include menstrual irregularities and breast tenderness.
Clascoterone is a topical antiandrogen that inhibits androgen receptor binding and reduces sebum production. It has mild side effects such as application site reactions and hypertrichosis.