
Ahmed N. M. Ghanem
NHS The UK and Mansoura University, Faculty of Medicine, Egypt
Consultant Urologist Surgeon- Retired Independent Investigator & Scientist, Free Lance Author, Dreamer & White Revolutionary in Science.
*Corresponding Author: Ahmed N. M. NHS The UK and Mansoura University, Faculty of Medicine, Egypt Consultant Urologist Surgeon- Retired Independent Investigator & Scientist, Free Lance Author, Dreamer & White Revolutionary in Science.
Received Date: June 20, 2023
Accepted Date: June 30, 2023
Published Date: July 28, 2023
Citation: Ahmed N. M. Ghanem. (2023) ““Hypovolaemia” with generalized edema, what is wrong? Time for new guideline recommendations on fluid therapy for shock resuscitation?.”, Aditum Journal of Clinical and Biomedical Research, 6(3); DOI: http;//doi.org/07.2023/1.10107.
Copyright: © 2023. Ahmed N. M. Ghanem. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
I read with great interest this recently published educational review article by Professors Fernando G. Zampieri, MD, PhD; Sean M. Bagshaw, MD, MSc; Matthew W. Semler, M D, MSc [1], identifying its limitations. I also read with great interest this recently published article by Professors Dull, R.O. and Hahn, R.G. [2]. The authors are commended on their reviews based on evidence from published reports that represent the current understanding of the condition and its scientific basis. The authors have faithfully and factually summarized the evidence based on published reports, including some of the commonly received errors and misconceptions on the scientific foundation [3] that identifying and correcting may help answer the vitally important question in the report's title [2]. I asked myself the very same question “What is wrong?” after attending the post-mortem examination of 3 patients who were killed by ARDS, complicating the TUR syndrome therapy back in 1981. It took me >40 years of hard, comprehensive, intensive, and profound scientific research to find the correct answer.
The authors acknowledge that Starling’s law represents the scientific foundation of the volume-pressure relationship of the vascular, capillary, and interstitial fluid compartments. It thus underlies and dictates the rules that govern fluid therapy in shock management. This is the subject on which the authors are among the top world authority. My research has demonstrated clearly and completely the substantial evidence that Starling’s law is wrong, and the correct replacement is the hydrodynamics of the porous orifice (G) tube [4,5]- that has been gathered in a new book [6]. This will revolutionize our understanding of the condition and related issues, particularly on the patho-etiology and management of ARDS. The hydrodynamics of the G tube in a surrounding chamber mimics the capillary-interstitial fluid (ISF) circulatory transfer (Figure 1).
shock; fluid therapy; ards; starling’s law; edema; hypovolaemia; hypervolaemia; vascular pressure; and volume
Introduction and text:
I read with great interest this recently published educational review article by Professors Fernando G. Zampieri, MD, PhD; Sean M. Bagshaw, MD, MSc; Matthew W. Semler, M D, MSc [1]. The review article is excellent and timely for it aimed at reviewing the evidence based on RCT and I thank them for their effort. However, it was a mistake to rely only on PubMed for their search which does not list all articles published in open-access journals. This has resulted in missing all the recent new substantial evidence on fluid therapy for shock, septic and others, and fluid resuscitation among which I reported >150 articles gathered later in 3 published books [6-8]. Off all my published articles only two were published in BJUI and Medical Hypothesis appear on PubMed search. The correct search engine to use is Google Scholar. A notable omission in the article is the scientific foundation of fluid therapy in septic and other types of shocks in acutely ill patients. There is no clear recommendation on how much fluid should be given to acutely ill patients with shock and when to stop to avoid the fluid creep that causes edema and ARDS in these patients as they did not mention Starling’s law on the causation of edema! That might be a good thing as it is now obsolete. Although I do understand and appreciate the seriousness of sepsis in destroying capillary-interstitial fluid circulation it is probably not responsible for the edema formation of ARDS, hence sepsis may be as innocent as the Wolf in Josef’s story. Sepsis is well covered and gets eradicated with the powerful antibiotics available today. Moreover, most acutely ill patients with massive, generalized edema and hypotension shock in ICU do not have evidence of sepsis. Furthermore, the condition may complicate fluid therapy for burns, trauma, acute pancreatitis, all known and newly recognized types of shock, and during prolonged major surgery. The fourth stage of fluid therapy that the authors called the “fluid removal stage” should be prevented or treated early- as mentioned later. Here is a brief summary or a mini-review of the new scientific foundation of fluid therapy for shock resuscitation and related issues.
I also read with great interest this recently published review article by Professors Dull, R.O. and Hahn, R.G. [5]. The authors are commended on this review based on evidence from published reports that represent the current understanding of the condition and its scientific basis for fluid therapy in the current clinical practice. The authors have faithfully and factually summarized the evidence based on published reports, including some of the commonly received errors and misconceptions on the scientific foundation [3] that identifying and correcting may help answer the vitally important question in the report's title [2]. I asked the very same question “What is wrong?” after attending the post-mortem examination of 3 patients who were killed by acute respiratory distress syndrome (ARDS), complicating the fluid therapy of the transurethral resection of the prostate (TUR) syndrome shock back in 1981. There was massive tissue edema with swollen vital organs and 3 litres of fluid in each peritoneal and pleural cavity. They were literally internally drowned by fluids infused for the resuscitation of shock. I asked the pathologist why he does not mention that in his report. His reply was: “Because it offends the treating physicians”! It took me >40 years of hard, dedicated, comprehensive, and intensive scientific research to find the correct answer. I knew then what was wrong, finished my physics experiments on the G tube by 1985, obtained my MD degree Thesis on understanding the TUR syndrome in 1988, and published my clinical prospective study in 1990 [9]. I reported the preliminary theory on capillary physiology in the Medical Hypothesis Journal in 2001 [4] but it took me >40 years to prove my new theory on the capillary-interstitial fluid circulatory transfer [10]. It is Galileo’s story all over again!
The authors acknowledge that Starling’s law represents the scientific foundation of the volume-pressure relationship of the vascular, capillary, and interstitial fluid compartments. It thus underlies and dictates the rules that govern fluid therapy in shock management. This is the subject on which the authors are among the top world authority. My research has demonstrated clearly and completely the substantial evidence that Starling’s law is wrong, and the correct replacement is the hydrodynamics of the porous orifice (G) tube [4,5]. The reported articles have been gathered in a completely new book [6]. This will revolutionize our understanding of the condition and related issues, particularly on the path-etiology and management of ARDS. The hydrodynamics of the G tube in a surrounding chamber mimics the capillary-interstitial fluid (ISF) circulatory transfer (Figure 1).
“Hypovolaemia and peripheral edema” [2] refer to the condition that affects acutely ill surgical patients presenting with any shock then suffer clinically with ARDS induced by excessive fluid therapy in whom there is massive volumetric overload with hypotensive shock (Hypovolaemia?) and massive fluid creep on the interstitial fluid space and vital organs causing generalized edema [11]. It complicates fluid therapy for shock resuscitation of burns, sepsis, haemorrhage, trauma, and acute pancreatitis, and during prolonged major surgery [12]. It initially presents and seamlessly occurs as volume kinetic or volumetric overload shock (VOS) [13], among new 13 scientific discoveries in physics, physiology, and medicine [14]. It has high morbidity and mortality and affects thousands of patients every year all over the world. Although there is hypotensive shock here, it is probably incorrect to assume “hypovolaemia” exists. In other words, and contrary to what is generally believed, hypotension is not synonymous with hypovolaemia. Frank-Starling’s law for the heart works with a physiological volumetric overload of <2 litres only, but with pathological VO it works paradoxically. It is a simple physics: if the cardiovascular system is overfilled to above its maximum capacity, the surplus fluid will simply spill into the ISF space!
Starling’s law has proved wrong on both of its hydrostatic and oncotic pressure forces [4,5] However, it continues to dictate the current faulty rules on fluid therapy in the management of shock. It thus misleads physicians into giving too much fluid during shock resuscitation [15]. More than 21 reasons were reported to show that Starling’s law is wrong [16]. The correct replacement is the hydrodynamic of the porous orifice (G) tube (Figure 1) that was built on the capillary ultrastructure anatomy of the precapillary sphincter [17] and a porous wall [18] that allows the passage of plasma proteins thus nullifying the oncotic pressure in Vivo. It follows that the extended Starling Principle is wrong, and a misnomer, and all the equations are also wrong [19]. Commonly received but erroneous concepts and laws represent fraud in modern science [20].
The clinical significance is that Starling’s law dictates the faulty rules on fluid therapy causing many errors and misconceptions that mislead physicians into giving too much fluid infusions of colloids and crystalloids for the resuscitation of shock [15] which both cause edema of ISF space and vital organs as well as “hypervolemia” with hypotension [13]. This shock is mistaken for septic shock or any known shock and is wrongly treated with further huge volume expansion, occurring with both liberal and conservative approaches of fluid therapy. This has been newly recognized as volume kinetic or volumetric overload shocks (VOS) [13]. Figures 2 and 3 show the volumetric overload and Table 1 shows its statistical significance (p=0.0007) in the path-etiology of the TUR syndrome and ARDS.
Volumetric overload (VO) inducing VOS is of 2 types: VOS 1 is induced by sodium-free fluids such as 1.5% Glycine, 5% Glucose, 3% Mannitol, and Sorbitol fluids that cause the TUR syndrome [9] which has a lifesaving therapy now [21]. It is predicted to reincarnate into ARDS after the shift to saline use as irrigant in endoscopic surgery [22]. VOS 2 is induced by sodium-based fluids of crystalloids and plasma proteins and causes ARDS and acute kidney injury (AKI) as part of the multiple organ dysfunction syndrome (MODS) with high morbidity and mortality [23]. VOS 2 may complicate VOS 1 or occur de novo. Volumetric overload shock induced by persistence to elevate CVP to a high level of 20-22 mmHg during shock resuscitation [24] is also based on the faulty Starling’s law and induces ARDS [23] that was originally reported by Ashbaugh et al in 1967 in which the dead patients had 12-14 Litres of fluid creep retained in their bodies [25]. In recent huge prospective multicentre clinical trial studies, fluid retention is 7-10 L in surviving ARDS patients [26].
I trust the respected authors, and invite the world authorities, to kindly fulfill their authority and responsibility by writing an update on the subject that summarises the results of my recently reported research for the awareness of the doctors’ readers and the undoubted benefit of their patients. Fortunately, the treatment is currently available which is hypertonic sodium therapy (HST) of 5% NaCl and 8.4% NaCo3 that simply saves lives [27]. This HST should be given as early and as quickly as possible while refraining from giving isotonic fluids of crystalloids and colloids when the retained fluid creep is 2-3 L or KG in weight. The HST induces massive diuresis when diuretics have failed. I also believe it is the right time to write new guidelines and recommendations on the use of fluid therapy for shock resuscitation [6].
Figures with legends:
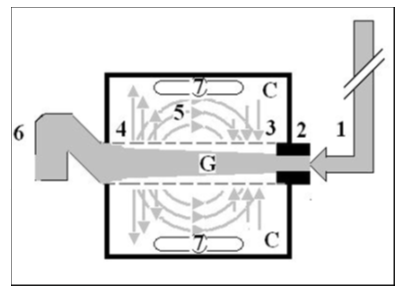
Figure 1: Shows a diagrammatic representation of the hydrodynamic of G tube based on G tubes and chamber C. This 38-years old diagrammatic representation of the hydrodynamic of G tube in chamber C is based on few photographs. The G tube is the plastic tube with narrow inlet and pores in its wall built on a scale to capillary ultra-structure of precapillary sphincter and wide inter cellular slit pores. The chamber C around it is another bigger plastic tube to form the G-C apparatus. The chamber C represents the ISF space. The diagram represents a capillary-ISF unit that should replace Starling’s law in every future physiology, medical and surgical textbooks, and added to chapters on hydrodynamics in physics textbooks. The numbers should read as follows:
1. The inflow pressure pushes fluid through the orifice
2. Creating fluid jet in the lumen of the G tube**.
3. The fluid jet creates negative side pressure gradient on the G tube’s wall causing suction maximal over the proximal part of the G tube near the inlet that sucks fluid into lumen.
4. The side pressure gradient turns positive pushing fluid out of lumen over the distal part maximally near the outlet.
5. Thus, the fluid around G tube inside C moves in magnetic field-like circulation (5) taking an opposite direction to lumen flow of G tube.
6. The inflow pressure 1 and orifice 2 induce the negative side pressure creating the dynamic G-C circulation phenomenon that is rapid, autonomous, and efficient in moving fluid and particles out from the G tube lumen at 4, irrigating C at 5, then sucking it back again at 3,
7. Maintaining net negative energy pressure inside chamber C that is always lower than the distal pressure at 6..
**Note: The shape of the fluid jet inside the G tube (Cone shaped), having a diameter of the inlet on right hand side and the diameter of the exit at left hand side (G tube diameter). I lost the photo on which the fluid jet was drawn, using tea leaves of fine and coarse sizes that runs in the center of G tube leaving the outer zone near the wall of G tube clear. This may explain the finding in real capillary of the protein-free (and erythrocyte-free) sub-endothelial zone in the Glycocalyx paradigm.
I also noted that fine tea leaves exit the distal pores in small amount maintaining a higher concentration in the circulatory system- akin to plasma proteins.
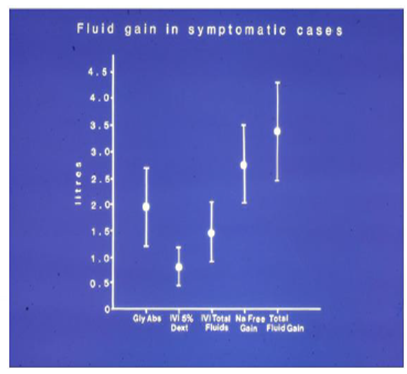
Figure 2: shows the means and standard deviations of volumetric overload in 10 symptomatic patients presenting with shock and Hyponatremia among 100 consecutive patients during a prospective study on transurethral resection of the prostate. The fluids were of Glycine absorbed (Gly abs), intravenously infused 5% Dextrose (IVI) Dext) Total IVI fluids, Total Sodium-free fluid gained (Na Free Gain) and total fluid gain in litres.
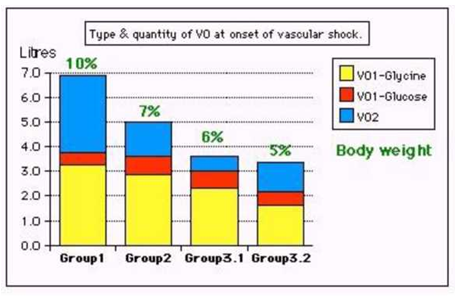
Figure 3: shows volumetric overload (VO) quantity (in litres and as percent of body weight) and types of fluids. Group 1 was the 3 patients who died in the case series as they were misdiagnosed as one of the previously known shocks and treated with further volume expansion. Group 2 were 10 patients from the series who were correctly diagnosed as volumetric overload shock and treated with hypertonic sodium therapy (HST). Group 3 were 10 patients who were seen in the prospective study and subdivided into 2 groups; Group 3.1 of 5 patients treated with HST and Group 3.2 of 5 patients who were treated with guarded volume expansion using isotonic saline.
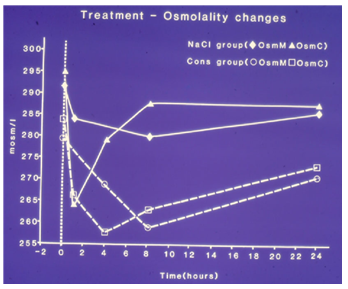
Figure 4: shows mean changes in measured serum osmolality (OsmM) and calculated osmolality (OsmC) in patients with the TURP syndrome comparing those infused with 5% hypertonic sodium (solid lines) and those treated conservatively (slashed lines). OsmC was calculated from the formula 2xNa+urea+glucose in mmol/l of serum concentration48 thus reflecting changes in serum sodium concentration. The vertical dotted line represents the start of operation (Time B) followed by C, C1, C2 (end of treatment) and D, respectively.
|
Parameter |
Value |
Std. Err |
Std. Value |
T Value |
P |
|
Intercept |
|
|
0.773 |
|
|
|
Fluid Gain (l) |
0.847 |
0.228 |
1.044 |
3.721 |
0.0007 |
|
Osmolality |
0.033 |
00.014 |
-0.375 |
2.42 |
0.0212 |
|
Na+ (C B) |
0.095 |
0.049 |
0.616 |
1.95 |
0.0597 |
|
Alb (C B) |
0.062 |
0.087 |
0.239 |
0.713 |
0.4809 |
|
Hb (C B) |
-0.282 |
0.246 |
-0.368 |
1.149 |
0.2587 |
|
Glycine (C B) |
-4.973E- 5 |
5.975E-5 |
-0.242 |
0.832 |
0.4112 |
Table 1: shows the multiple regression analysis of total per-operative fluid gain, drop in measured serum osmolality (OsmM), sodium, albumin, Hb and increase in serum glycine occurring immediately post-operatively in relation to signs of the TURP syndrome. Volumetric gain and hypoosmolality are the only significant factors. (Reproduced with the permission of author and editor of BJU Int. from reference 9).
Conflict of interest: None declared.
Funds received: None declared.
Declarations:
Ethical Approval:
Is not applicable. I consent to participate in and consent to publish this article.
Availability of data and materials:
The datasets used can be accessed from the given references of published articles and books.
Acknowledgment:
I thank Mr. Khaled AN Ghanem, MBChB, MRCS for constructive criticisms and helpful comments on this article. I would like to thank the editors of JAMA for allowing a free download of the article and for helping to spread the new knowledge in this article by accepting and reporting it.
Abbreviations:
ARDS Acute Respiratory Distress Syndrome
TUR Syndrome Transurethral Resection of the Prostate Syndrome
G Tube Porous Orifice Tube
ISF Capillary-Interstitial Fluid
VO Volumetric Overload
VOS 1 Volumetric Overload Shock Type 1
VOS 2 Volumetric Overload Shock Type 2
AKI Acute Kidney Injury
MODS The Multiple Organ Dysfunction Syndrome
CVP Central Venous Pressure
NaCl Sodium Chloride
NaCo3 Sodium Bicarbonate
HST Hypertonic Sodium Therapy