Aditum Journal of Clinical and Biomedical Research
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2993-9968 | Journal DOI: 10.61148/2993-9968/AJCBR
Rubel Andrés Lafaurie Noriega1*, Jorge Eduardo Montes Argumedo2, William Pinzón Gallardo3, María Fernanda Ramos Sánchez4, Juan Luis Pareja Rodríguez5, José Miguel Gutiérrez Gallego6, Rafael Alfonso Reyes Monge7, Mario Enrique Sayas Herazo8
1Physician Epidemiologist, Universidad Autónoma de Bucaramanga, Colombia. 0000-0002-2606-0621.
2General Physician, Universidad del Norte, Colombia.
3General Physician, Universidad Surcolombiana, Neiva.
4Physician Surgeon, Universidad Nacional de Colombia.
5General Physician, Universidad Privada Antenor Orrego, Perú.
6General Physician, Fundación Universitaria Autónoma de las Américas, Colombia. 0000-0001-5443-7935.
7Specialist in Emergency Medicine, Universidad Michoacana de San Nicolás de Hidalgo. 0000-0002-9201-7250
8General Physician, Corporación Universitaria Rafael Núñez, Colombia.
*Corresponding Author: Rubel Andrés Lafaurie Noriega, Physician Epidemiologist, Universidad Autónoma de Bucaramanga, Colombia. 0000-0002-2606-0621.
Received: November 22, 2021
Accepted: December 23, 2021
Published: January 05, 2022
Citation: Rubel Andrés Lafaurie Noriega, Jorge Eduardo Montes Argumedo, William Pinzón Gallardo, María Fernanda Ramos Sánchez, Juan Luis Pareja Rodríguez, etc.al. (2021) “Utility of Corticoids in Septic Shock.”, Aditum Journal of Clinical and Biomedical Research, 4(1); DOI: http;//doi.org/01.2022/1.1067.
Copyright: © 2022 Rubel Andrés Lafaurie Noriega. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Septic shock (SS) is very prevalent today, ranking among the top 10 causes of death worldwide due to its high rate of systemic complications. Due to its pharmacological profile, it has been proposed on several occasions that the use of steroids in SS may associate a beneficial effect on patient survival. Numerous studies have been carried out in order to demonstrate their role, considering both the pharmacodynamics and pharmacokinetics of corticosteroids, as well as their final effects in terms of mortality, reversibility of shock, and possible adverse effects. The objective of this article is to discuss, based on current evidence, the role of these drugs in said pathology in order to define the different scenarios in which the patient can benefit from them.
Introduction:
Despite technological advances and the development of both diagnostic and therapeutic stratifications, the mortality rate from sepsis has not changed in the last 40 years, even sepsis has increased in the last decades.
According to the Pan American Health Organization, infectious diseases are the leading cause of death worldwide. Of the 53 million people reported with infectious diseases, 18 million die annually and 1,400 daily, representing 30 to 50% mortality. [1] In the United States in 2002 it reported 750,000 cases of severe sepsis annually and by 2012 these are close to a million, of which 215–225,000 were fatal, comparable to the number of deaths from acute myocardial infarction (AMI) and cerebrovascular disease. Every 3 to 4 seconds someone dies from sepsis and within a year it causes more deaths than prostate cancer, breast cancer, HIV, and even more than all of these diseases combined. [2]
Septic shock is defined as sepsis-induced hypotension despite adequate fluid therapy. [3] Its initial management, based on the administration of the indicated antibiotic therapy, as well as the assessment of the patient's hemodynamic compromise and resuscitation with fluid therapy and vasopressors, is a fundamental part of the approach. [4]
In recent years, scientific evidence has been essential for the development of new recommendations and clinical guidelines in order to improve the management of the septic patient. These recommendations include the administration of corticosteroids, where these drugs have exceeded only endocrine use and are used as adjunctive treatment [5,6]. Glucocorticoids are drugs with anti-inflammatory, antiallergic and immunosuppressive effects, which are derived from hydrocortisone or cortisol; hormones produced by the adrenal cortex, essential for a correct adaptation to stress. They are drugs that protect the body from the consequences that an indiscriminate inflammatory response can develop.
Currently, glucocorticoids are considered as immunoregulators and not as immunosuppressants, since they do not cancel the secretion of some cytokines, but instead increase the expression of coreceptors for cytokines and optimize the response of T11 lymphocytes. [6] On the other hand, recent studies on the use of corticosteroids in this type of patients, and their possible effect to reduce mortality and improve prognosis, show controversial results, since corticosteroids are associated with immunosuppression and risk of superinfection in septic patients. [7]
That is why a systematic review was proposed, in order to find out if there is scientific evidence that demonstrates a beneficial effect of corticosteroid treatment in patients with severe sepsis or septic shock, as well as to establish, if positive, if it has been demonstrated a more convenient management, according to the evidence, of corticosteroids in this pathology.
Methodology:
Design:
The design of the study was that of a systematic review of the evidence in the scientific literature on the efficacy of the administration of corticosteroids in patients with septic shock and severe sepsis with the premise of responding to the stated objectives.
The literature search took place between October and November 2021, delving into various bibliographic databases in order to obtain information and review previous studies on the exposed topic. The databases used were Pubmed-Medline, Web of Knowledge (WOK) and SCOPUS, in which the search strategies differed depending on the source used. The keywords and Boolean operators used were "severe sepsis" OR "septic shock" AND "corticosteroids" AND "mortality" described through DeCS (Descriptors in Health Sciences). In order to obtain a greater update on the matter, the articles published in the last 20 years were set as a temporary filter for the search.
Results:
The American College of Chest Physicians and the Society of Critical Care Medicine in 1991 convened a consensus conference, the objectives of which were aimed at defining conceptually under the term of sepsis the progressively harmful processes that go from the Systemic Inflammatory Response Syndrome to the Multiorgan Dysfunction Syndrome. In this international consensus conference that was chaired by Roger Bone, important definitions were approved that allowed the unification of the terminology used. Later, in 2001, the international consensus conference on the definitions of sepsis was held and the maintenance of the 1991 Bone criteria was approved by all its participants. In 2012, their validity was fully reaffirmed. The definitions analyzed were the concept of infection, bacteremia, SIRS (Systemic Inflammatory Response Syndrome), sepsis, severe sepsis, severe high-risk sepsis, septic shock, and multi-organ dysfunction syndrome (MODS). [9]
Thus establishing the following concepts:
Sepsis: systemic response of the organism to SIRS infection as a consequence of a suspected, proven, documented, demonstrated infectious process.
Septic shock: It is one of the most feared medical conditions with a very high mortality, from the functional point of view it is defined as the failure of the circulatory system, that is, of the heart as a pump and the entire vascular bed in function of distributing the blood, it is an unbalanced condition between oxygen supply and demands at the cellular level
Multi-organ dysfunction syndrome: Acute process characterized by a slow, gradual, progressive, continuous, sequential and simultaneous deterioration of the functions of organs and organ systems, which generally begins with respiratory failure, followed by dysfunction of the nervous, liver, intestinal, renal and other organs that are not necessarily involved in the primary disease, nor do they appear in a predetermined order. [9,10]
Next, we have that steroids are a group of drugs related to hormones produced in the adrenal cortex. Widely used in the clinic for its anti-inflammatory and immunosuppressive properties. They are a fundamental part of the treatment of diseases in which there is an inflammatory component, some infectious diseases are included. Although their mechanism of action is not known in detail, it is known that they exert their effects by acting on different effector cell lines of the immune system, reducing the production of antibodies and cytokines. For this reason, among its side effects, the increased susceptibility to infections stands out, which requires careful consideration of the risk / benefit ratio. [11]
Corticosteroids are known to play an important role in modulating the inflammatory response through the activation of the corticosteroid receptor alpha, however, their activity in sepsis is not limited to inhibiting the inflammatory response mediated by NFkB, (nuclear factor kappa), but rather it also has cardiovascular effects. They induce sodium and water retention through corticosteroid and aldosterone receptors, increase peripheral vascular resistance, improving vascular sensitivity to alpha adrenergic agonists in a matter of minutes to hours, without altering pulmonary circulation and cardiac index, in addition to Moderate doses of hydrocortisone increase capillary density and perfusion in patients with septic shock (approximately one hour after administration) by generating upregulation in endothelial NO levels. [12]

Figure 1A: Physiological effect of corticosteroids.
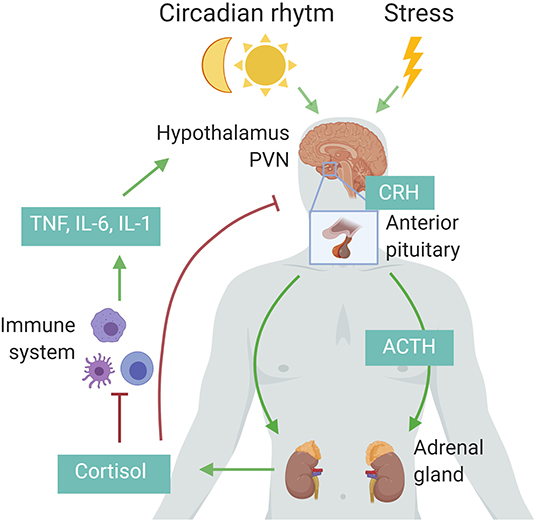
Figure 1B: Effect of corticosteroids in septic shock.
Effects of Corticosteroids in Septic shock:
Steroids can be useful in patients with septic shock, in whom there is demonstrated adrenal insufficiency with an insufficient elevation of serum cortisol when stimulated with ACTH (Adrenocorticotropin). They increase myocardial contractility, heart rate, cardiac output, ejection fraction, minute volume, splanchnic and renal flow. They block the synthesis of nitric oxide. They play an important role in regulating the synthesis of adrenergic receptors; This fact acquires great importance in patients in whom treatment with high-dose catecholamines is added to the hyperadrenergic state of the situation. [13]
Regarding the mechanisms by which steroids are beneficial in sepsis. Three pillars were analyzed: anti-inflammatory effect, increased sensitivity of adrenergic receptors, vascular tone and blood pressure, and lastly the effect on relative adrenal dysfunction. In addition to the already known anti-inflammatory effect, the participation of steroids in the activation of the nuclear factor Kappa B inhibitor has been explained. [14]
In the presence of certain factors, different types of stress, endotoxins, proinflammatory cytokines, hemorrhage, hypovolemia, hypoxia, hyperoxia, which activate NF-KB. NF-KB is a powerful signal transcriptionist for the production of pro-inflammatory cytokines, it is a dimeric protein located in the cell cytoplasm, linked to a protein that keeps it blocked and inactive (INF-KB). Activation of NF-KB leads to phosphorylation of the inhibitory protein. Steroids modulate transcription factors through two ways: they bind to their cytoplasmic receptor and enter the cell nucleus, once in the nucleus they are able to bind directly to NF-KB block its action and activate the inhibitory protein of NF- KB, inhibit the transcription of signals for the production of pro-inflammatory cytokines. [15]
The anti-inflammatory activity of steroids on the nervous system is given because it reduces cerebral edema, reduces intracranial pressure and reduces the permeability of the blood-brain barrier. Hence, the main indications for these are in high-risk CNS sepsis: signs of cerebral edema on CT, signs of elevated intracranial pressure, neurological focality, or increased cerebrospinal fluid (CSF) outlet pressure. [16]
Another mechanism that steroids have is that, by inhibiting nitric oxide, the sensitivity and reactivity of adrenergic receptors is synthesized and increased, they improve hemodynamics, vascular sensitivity to vasopressor drugs, which allows decreasing doses of catecholamines, decreasing the duration of shock, multi-organ dysfunction and therefore mortality. [17]
To conclude, we have The third pillar that supports the use of steroids in sepsis is relative adrenal dysfunction. Relative adrenal insufficiency refers to the fact that in a situation of maximum stress (noxa septic), the hypothalamic pituitary adrenal axis is stressed, therefore, the available plasma levels of cortisol are at the maximum, those that are impaired, altered are not the same plasma levels of available cortisol but the possibility of the adrenal reserve to respond to a new situation of additional stress. In fact, the patients who do better are those with an adrenal response. [18]
Discussion:
Published studies on the use of steroids in severe sepsis and septic shock show that in 1963 the first prospective randomized studies with the use of steroids in supraphysiological doses appeared. The controversy then arises as to whether or not to use these drugs as a therapeutic weapon against severe sepsis and septic shock. From then on, the debate would continue in international forums and the medical literature would be invaded by studies, some in favor and others against their use. An example would be the study by Shumer et al, in 1976, which included 172 patients to whom steroids (methylprednisolone, dexamethasone or placebo) were administered in a single dose at the beginning of the clinical picture, thereby reducing mortality at 28 days. . [19]
Subsequently, many studies were developed, among the most important in SS and steroid management, we can cite the randomized controlled trials carried out by Annane in 2002 and Sprug in 2008; where both show contradictory results, due to the fact that although they coincide in the fact that there is a greater reversibility of SS when corticosteroids are used, the first author concludes that there is a decrease in mortality while the second indicates that the itself is not significantly impacted. [19]
Next, Annane et al. published another review in 2009, this included a total of 17 randomized and 3 quasi-randomized studies, twelve of which corroborated a decrease in short-term mortality and an improvement in reversibility of SS in patients with SS, after 28 days after receiving low doses of steroids, defining them as those below 300mg / d. [20]
On the other hand, in a cohort study published by Funk et al.14, it was evaluated whether there was a benefit in patients diagnosed with septic shock who received low doses of corticosteroids within the first 48 hours after their diagnosis, comparing them with other subjects with the same diagnosis who were not treated with corticosteroids. 6663 patients were recruited, of whom 2031 received low-dose intravenous corticosteroids (150-300 mg / day), and 4632 subjects who did not receive such treatment. A greater survival benefit was obtained from the use of corticosteroids in patients with higher APACHE II, where the reduction in mortality was 5.2%. [21]
A meta-analysis of 12 randomized, double-blind, placebo-controlled clinical trials in 2009 in patients with sepsis secondary to severe pneumonia, which showed a reduction in mortality in patients treated with low-dose corticosteroids (300 mg per day hydrocortisone for 7 days) [22]
Conclution:
The early initiation of corticosteroids influences their efficacy, therefore, in patients with criteria for treatment with corticosteroids, it is advisable to administer said therapy as early as possible and at low doses, which is the most scientific evidence shows. Candidate patients for such treatment are those with greater severity and who do not respond to resuscitation with fluids and vasoactive drugs, the next step in their treatment being corticosteroid therapy. the results have been inconclusive. Several studies show improvement in the reversibility of septic shock, however, other parameters such as mortality have not shown significant improvement, ending treatment with corticosteroids in patients who develop septic shock should not constitute a routine action, since if they respond positively to resuscitation with fluids and vasoactive drugs, the administration of corticosteroids does not suppose benefits in its state but on the contrary, it accentuates the already existing damages.
Interest Conflict: The authors have declared no conflict of interest.