Aditum Journal of Clinical and Biomedical Research
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2993-9968 | Journal DOI: 10.61148/2993-9968/AJCBR
Rhonald Gómez Caballero1*, Rubel Andrés Lafaurie Noriega2, Diana Carolina Caballero Negrete3, Julian Serrano-Giraldo4, Jorge Eduardo Montes Argumedo5, Galber Manuel Echeverria Camargo6, Armando Hongming Yee Acendra7, Ader Andrés Vergara Álvarez8
1General Physician, Universidad de Ciencias Ambientales y Aplicadas, Bogotá, Colombia.
2Physician Epidemiologist, Universidad Autónoma de Bucaramanga, Colombia. 0000-0002-2606-0621
3General Physician, Universidad Libre de Barranquilla, Colombia.
4General Physician, Pontificia Universidad Javeriana de Bogotá, Colombia.
5General Physician, Universidad del Norte, Colombia.
6General Physician, Universidad libre, Barranquilla, Colombia.
7General Physician, Fundación Universitaria San Martín de Barranquilla, Colombia.
8General Physician, Universidad Libre seccional Barranquilla, Colombia.
*Corresponding Author: Rhonald Gómez Caballero, General Physician, Universidad de Ciencias Ambientales y Aplicadas, Bogotá, Colombia.
Received: November 22, 2021
Accepted: December 23, 2021
Published: January 05, 2022
Citation: Rhonald Gómez Caballero, Rubel Andrés Lafaurie Noriega, Diana Carolina Caballero Negrete, Julian Serrano-Giraldo,and Jorge Eduardo Montes Argumedo, etc.al. (2022) “Risk Factors Associated with Infections by Resistant Multi-Drug Bacteria in Critical Patients with Kidney Substitution Therapy.”, Aditum Journal of Clinical and Biomedical Research, 4(1); DOI: http;//doi.org/01.2022/1.1066.
Copyright: © 2022 Rhonald Gómez Caballero. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Chronic kidney failure (CKD) or chronic kidney disease (CKD) is a public health problem worldwide, the number of patients has been increasing both in developed and developing countries without discrimination of their age, reason Therefore, the need to resort to dialysis or hemodialysis procedures or, failing that, kidney transplantation is increasing, the latter being the most common option for patients with chronic kidney disease, both in terms of survival and quality of life. Therefore, it is essential to identify the risk factors associated with hospital infection that can affect this population, since a constant evolution in the last 40 years of nosocomial infections has been observed, being important to highlight the infection by multidrug-resistant bacteria that they can be more life-threatening for these patients. The recognition of these risk factors is the basis of the problem whose resolution has a positive impact on reducing the incidence of Infections Associated with Health Care.
Introduction:
Chronic kidney disease (CKD) is considered to be irreversible kidney damage that can progress to end-stage kidney disease, characterized by a gradual decline in kidney function, with an increase in serum urea and creatinine [1]. Undoubtedly, it is a public health problem that affects many patients without age discrimination, therefore, as a consequence, the need to resort to renal replacement therapy procedures is increasing, which is why it is useful to perform a renal replacement therapy. Review of the literature to identify risk factors associated with multidrug resistant bacteria (MDR) infections in critically ill patients with renal replacement therapy.
There are different types of renal replacement therapies that can be seen in Figure 1. In the final stage of the disease, the main treatment modalities are usually hemodialysis, peritoneal dialysis and kidney transplantation. Kidney transplantation is the most common option for patients with chronic kidney disease, both in terms of survival and quality of life [2]. Of all these, it has been described that hemodialysis brings with it risks of infectious and non-infectious adverse reactions, both due to factors inherent to the host and those derived from the procedure. Among the factors inherent to the host; The most common chronic diseases such as diabetes, heart disease and time on hemodialysis have been described, on the other hand, it is important to take into account host factors due to the constant contribution that it has to increase the patient's comorbidities due to immunosuppression than pathologies chronicles produce. Among the factors associated with the procedure are those related to the hemodialysis technique, type of monitor, type of vascular access, training and experience of the team in charge; and some direct care techniques, among others. Everything mentioned above leads to the appearance of infections associated with health care, which currently due to antibiotic resistance there are so-called MDR bacteria, which is an even more serious problem that can increase mortality [3].

Figure 1: Types of renal replacement therapies
In general, infections associated with health care are acquired inhospital institutions as well as in outpatient clinics. They are characterized by being the most frequent event, which represents high costs for health entities in such a way that they impact on individual and family living conditions. These infections represent more than 90% of infections, highlighting pneumonia and catheter-associated bloodstream infections, they are attributed 60% of mortality, being the eighth leading cause of death in the United States. [4] Therefore, bacterial multidrug resistance is a worldwide problem that requires constant vigilance and control to limit and mitigate it. At present, the hospital environment is a favorable place for the emergence of bacterial resistance due to the high bacterial concentration and the constant use of antibiotics, which is why the appearance of multiresistant endemic strains is frequent in hospitals [5].
In Latin America, in relation to infections caused by resistant bacteria, resistance is a limitation for the adequate treatment of infected patients both in the hospital area and in the community. The high rates of antibiotic resistance reported in healthcare-associated infections are a major threat, including methicillin-resistant Staphylococcus aureus (MRSA), Extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBL), Pseudomonas aeruginosa, and Acinetobacter baumannii resistant to carbapenems (Table 1) [6]. In Latin America, there were higher levels of antimicrobial resistance compared to the United States and Europe. [7]
|
Table 1: Multidrug-resistant bacteria associated with health care |
|
Methicillin resistant Staphylococcus aureus (MRSA) |
|
Extended-spectrum β-lactamase-producing Enterobacteriaceae |
|
Pseudomonas aeruginosa |
|
Acinetobacter baumannii resistant to carbapenems |
Therefore, factors related to multi-resistant bacterial infections include prolonged hospitalization, chronic diseases, surgical interventions, ICU admission, insertion of invasive devices, non-compliance with biosafety measures, and inappropriate use of antibiotics [8]. Although, these have been divided into intrinsic and extrinsic risk factors as shown in Figure 2. Of all the risk factors mentioned, there is undoubtedly a lot of association with patients who undergo renal replacement therapy because, generally , any type of these therapies subject the patient to invasive procedures, where the hygiene of medical implements and staff plays an important role, in addition, the stay of these patients in the hospital is constant and their partial or total loss of function Adding to it the immunosuppressive treatment makes them the target of nosocomial infections due to multidrug-resistant bacteria, in fact, these infections are an important cause of morbidity and mortality in the most serious stages of the disease, more specifically after transplantation, although the use of prophylactic antibiotics at the time of surgery, these risks have notably decreased. Infection occurs in up to 30% of kidney transplant recipients during the first three months after transplantation [9].
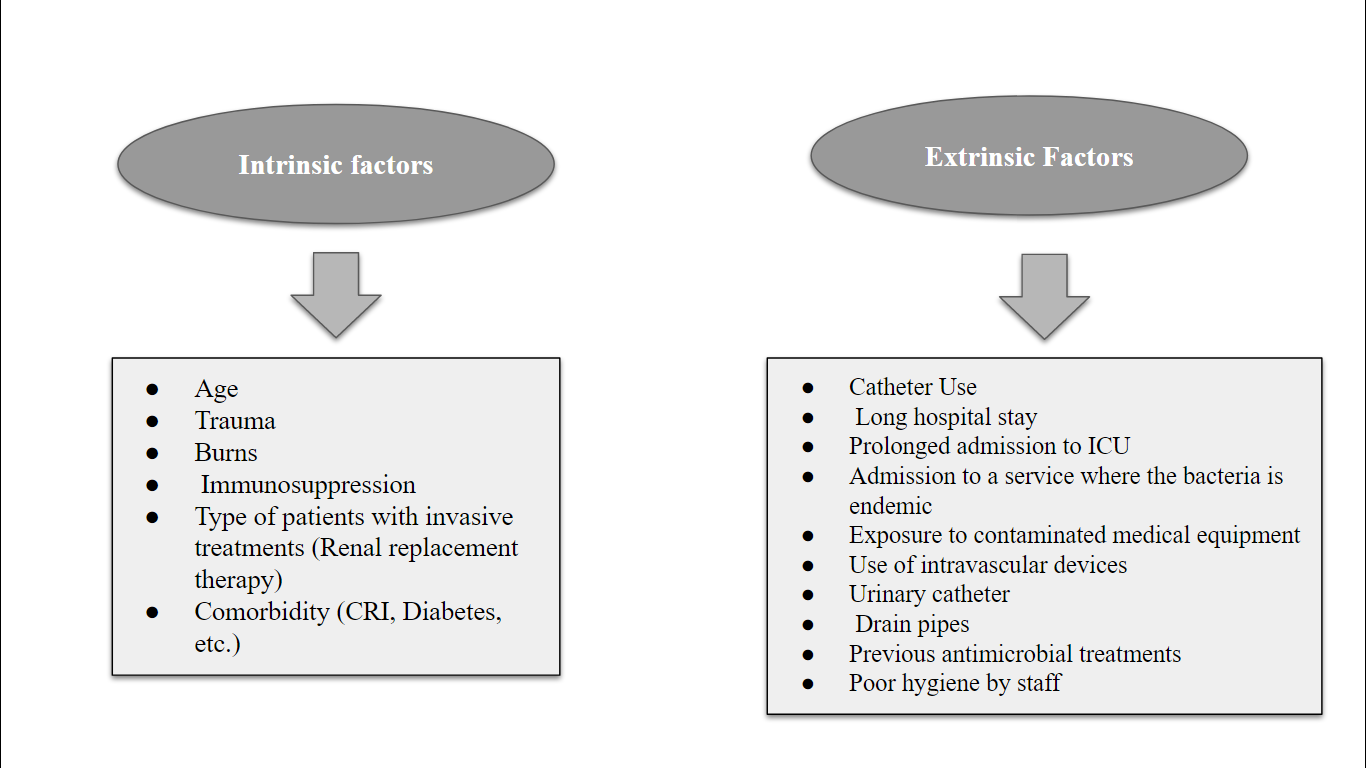
Figure 2: Risk factors associated with infections by multidrug resistant bacteria.
Materials and Methods:
In this review article, a detailed bibliographic search of information published since 2014 was carried out, in the databases pubmed, Elsevier, scielo, national and international libraries. We use the following descriptors: infection, risk factors, renal replacement, multidrug-resistant, therapy. The data obtained oscillate between 2 and 15 records after the use of the different keywords. The search for articles was carried out in Spanish and English, more relevant published studies were used.
Results:
The articles used collect the results of different studies that indicate that the risk factors for developing multidrug-resistant infections include those that were present before transplantation, in the recipient or donor, and those that appear as a consequence of immunosuppressive treatment and the surgical act itself. The urinary tract being the most likely area to develop infection in kidney transplant patients. Increasing the risk in diabetic patients. The European Society of Urology recommends that all patients with stage 5 or stage 4 chronic kidney disease, with glomerular filtration rates <15 ml / min and 15-30 ml / min respectively, with progressive disease likely to require replacement therapy kidney disease within six months should be considered for transplantation [10]. Subsequently, bacterial resistance is becoming a public health problem of increasing magnitude, which is why patients who require renal replacement therapy are subjected to interventionism either for implantation and management of hemodialysis catheters, or manipulation of arteriovenous fistulas or catheters peritoneal areas that are access routes for colonization and infection by various microorganisms. Therefore, a study identified the risk factors related to Gram negative colonization and found results in patients with a history of ICU stay OR: 36.46, acute renal failure OR: 6.23, dialysis OR: 10.80 mechanical ventilation OR: 17.5, catheterization bladder OR: 14.3, use of carbapenems OR: 18.52, quinolones OR17.30, cefepime OR: 28.05, glycopeptides OR: 19.1; metronidazole OR: 4.17, p: 0.03, colistin OR: 12.1, linezolid OR: 7 (11). This means that the preventive measures of modern medicine of surgical techniques, immunosuppression protocols, follow-up periods and the administration of antimicrobials are not enough. Post-kidney transplantation urinary tract infection continued to be a major public health problem worldwide. A cross-sectional study conducted in a hospital has shown that significant bacteriuria was found in 11/74 (14.9, 95% CI = 8.2 to 24.7) transplant recipients, which was relatively low. However, they found Escherichia coli 2 (18.2%), Staphylococcus aureus 2 (18.2%) as the most prevalent bacteria, Acinetobacter spp 2 (18.2%), Enterococcus spp. 2 (18.2%), coagulase negative staphylococci 2 (18.2%) followed by Porteus mirabilis 1 (9.1%). Of which 80% were resistant to ciprofloxacin, chloramphenicol and trimethoprim / sulfamethoxazole [12]. In particular, the evolution of immunosuppressive therapy has reduced the rates of acute graft rejection, but the propensity to develop post-transplant infections has increased, so studies suggest adequate perioperative prophylaxis in high-risk patients targeting the potential pathogens they produce. Surgical site infection in kidney and / or pancreas transplant recipients and a reduction in cold ischemia may be beneficial in reducing these SSIs [13]. Freire et al. Diagnosed urinary tract infection in 178 (23.9%) of 781 kidney transplant recipients, who developed 352 episodes of UTI. In addition, 44.6% of UTI cases were caused by multidrug-resistant bacteria and identified as risk factors, diabetes mellitus, urological disease as a cause of end-stage renal failure, insertion of a ureteral stent, use of carbapenems, and delayed graft function [14]. Attias et al. Retrospectively analyzed a single-center cohort of transplanted adult kidney allograft recipients and found that viruses were the main cause of opportunistic infections (n = 54, (10%)), followed by fungi (n = 15 (3%)), parasitic (n = 6 (1%)) and bacterial (n = 5 (0.9%)) infections. Of the bacterial infections, 40% were tuberculosis, 40% were nocardiosis, and 20% were disseminated infection by atypical mycobacteria [15]. A study published in 2018 reports that poor kidney function at the time of hospital admission is associated with a greater probability of having infection by multi-resistant organisms, which are defined as specific pathogens (Staphylococcus aureu s, Enterococcus spp., Enterobacteriaceae, Pseudomonas aeruginosa and Acinetobacter spp.). In addition, from a total of 94,445 records of microbial cultures, 7,288 first positive cultures were selected that coincided with the diagnosis of infection. Among them, 5,028 (68.9%) were possible MDROs. The odds of MDRO infections were 19% and 41% higher in those with eGFR between 30-59 ml / min / 1.73 m 2 (adjusted odds ratio, AOR): 1.19, 95% CI: 1.02-1.38, P = 0.022) and eGFR <30 ml / min / 1.73 m 2 (AOR: 1.41, 95% CI: 1.12–1.78, P = 0.004), respectively [16]. In a single prospective study trick in the ICU of the China Japan Friendship Hospital where there were 604 cases (36.12%) colonized by multi-resistant organisms, of which 62 cases (3.71%) were colonized with Staphylococcus aureus resistant to methicillin, 529 (31.64%) were colonized with extended spectrum. Enterobacterias β-lactamasa, 7 (0,42%) were colonized with multi-resistant Acinetobacter baumannii, and 6 (0.36%) were colonized with multi-resistant Pseudomonas aeruginosa [17]. This suggests that intensive care unit patients, and particularly those with acute kidney injury, have a high risk of developing nosocomial bloodstream infections due to multidrug resistant strains, which is confirmed in a study that included 1330 patients with acute kidney injury undergoing renal replacement therapy, 92 had microbiological evidence of nosocomial bloodstream infections (57/92, 62% due to a multidrug resistant microorganism) [18]. Therefore, surgical site infections and urinary tract infections are complications of renal function replacement therapy. Being in evidence once again, when diagnosing with infection in the surgical site (SSI) in 7.25% (19/262) of the patients. Of nineteen SSI patients, two (10.5%) were diagnosed with organ-specific SSI, which ultimately led to graft loss; six (31.5%) developed deep incisional SSIs; and eleven (58%) developed superficial incisional SSIs. In addition, the following risk factors for SSI development were found as determinants: kidney from donors with extended criteria, cold ischemia time of more than 30 hours, surgical procedure time greater than 200 min, confirmed diabetes in recipients. , a recipient's body mass index greater than 27 kg / m, and the appearance of delayed graft function [19].
Discussion:
In recent years, despite the effectiveness of kidney transplantation, and the evident improvement in the quality of life of patients undergoing kidney replacement, the development of various infections of bacterial origin, mediated by resistant microorganisms, that is, those that They present resistance to 3 or more groups of antibiotics, constitute a severe complication in the patient, which leads to a compromise both of the transplanted organ and the systemic and general health of the patient, so that in the long term it can cause death.
According to various studies carried out, it is estimated that bacterial infections constitute more than 70% of postoperative infections, the most frequent being urinary infection, surgical site infection and acute lung disease, in addition, the most frequent etiology is enterobacteria predominantly Escherichia coli and Klebsiella spp., followed by Pseudomonas aeruginosa and Enterococcus spp. [20]
Due to the large number of cases presented of kidney transplantation with an ongoing bacterial infection, it is important to determine those risk factors that increase the probability of it, in order to establish preventive measures that reduce this risk and in turn allow the correct surgical procedure. Taking into account that the main bacterial foci are the hospital environment, the use of catheters, the operating room, the equipment used in the procedure, etc., it is important to be clear that the entry of this bacterium into the body can easily occur, however, Its resistance lies in the constant use of antibiotics without a prescription and without necessity, therefore, the drug does not have an effect on it, so that the infection continues its course.
One of the main resistance mechanisms of these bacteria is the production of extended spectrum beta-lactamases (ESBL), which are enzymes capable of inactivating, in addition to penicillins and first and second generation cephalosporins, oximino-cephalosporins and aztreonam [21], so that, when using these drugs, these bacteria will have the ability to eliminate their therapeutic effect. Therefore, Moreno et al., In their bibliographic review, conclude that the risk factors for developing an infection by ESBL-producing bacteria are prior antibiotic treatment, double kidney and pancreas transplantation, the requirement for post-transplant dialysis and the presence of of urinary tract obstruction. The development of this complication is associated with a worse prognosis for the graft and the patient. Another important fact is that multi-drug resistant strains have to be treated with second or third line antibiotics, which generally have considerable disadvantages, highlighting the higher incidence of adverse effects (renal toxicity in the case of aminoglycosides and colistin, neurological toxicity with colistin, etc.) and the lower availability of oral formulations that entails prolongation of hospital stay. If empirical treatment does not effectively cover these microorganisms, mortality may rise. [22]
For their part, Mendez et al., In their retrospective study, in which an exhaustive review of 304 patients who underwent kidney transplantation between 2002 and 2011, concluded that the risk of UTI, consequently, is multifactorial and it is determined by the interaction of the host's clinical condition, pathological agents, and anatomical abnormalities [23]. Furthermore, the indiscriminate use of antibiotics represents the main cause of resistance.
Due to the importance of treating these types of patients, Lan recommends first-line combination therapy for patients diagnosed with a severe infection caused by carbapenemase-producing microorganisms. Combination treatment will be performed with 2 fully active antimicrobials (including colistin, tigecycline, aminoglycoside or fosfomycin, and meropenem) if the MIC (minimum inhibitory concentration) is <8 mg / l. [24]
Therefore, the use of antibiotics without a prescription is a global health problem that affects the general population, because their consumption leads to resistance, which will affect the health of the patient in the long term, since during the course of an infection, such as those produced by different causes after a surgical procedure, mainly organ transplantation, they will have the ability to systemically affect the body, which increases mortality rates and decreases the effectiveness of the procedure, being necessary that health personnel and international organizations inform the civil population about the correct use of this type of medication as a preventive action, in order to reduce its unnecessary use and therefore, resistance to the same.
Conclusion:
During the course of chronic kidney disease or kidney failure, it becomes necessary to implement different measures that seek to improve the quality of life of patients and in turn reduce the severity of the disease, therefore, kidney transplantation constitutes a one of the most effective and currently used measures.
Due to the high degree of exposure of patients to different bacterial foci, such as the constant use of catheters, the lack of asepsis in certain instruments used during the surgical procedure, the operating room, the stay inhospital spaces, etc. The rates of infections secondary to this have increased, affecting both the transplanted organ and the general health of the patient. However, it has been shown that most of these infection-causing bacteria are resistant to different types of antibiotics, which is why it is determined that the main risk factor of suffering an infection by multidrug-resistant bacteria is the excessive and continuous use of antibiotics. This is why it is necessary for international health entities to be in charge of educating and guiding the general population on the correct use of this type of drugs, in order to reduce their inappropriate use and therefore the resistance of certain bacteria that in the long term cause severe complications in this type of procedure.