
Mounir Hmidi1*, Hamza Belatik1, Mohamed Sinaa 2, Ali Elboukhari 1, Karim Nadour 2
1Department of Otorhinolaryngology-Head and Neck Surgery, Military Hospital Meknes, Morocco.
2Department of Pathology, Military Hospital Meknes, Morocco.
*Corresponding Author: Mounir Hmidi, Department of Otorhinolaryngology-Head and Neck Surgery, Military Hospital Meknes, Morocco.
Received: June 24, 2021
Accepted: June 29, 2021
Published: July 07, 2021
Citation: Mounir Hmidi, Hamza Belatik, Mohamed Sinaa , Ali Elboukhari and Karim Nadour. (2021) “ Intravascular Papillary Endothelial Hyperplasia: An Unusual Cause of Submandibular Swelling.”, J Oncology and Cancer Screening, 3(1); DOI: http;//doi.org/06.2021/1.1031.
Copyright: © 2021 Mounir Hmidi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Intravascular Papillary Endothelial Hyperplasia (IPEH) also known as Masson’s tumor is an unusual, non-neoplastic vascular lesion commonly found on the head, neck, and extremities. Histologically, it is characterized by a papillary proliferation of endothelial cells forming vascular channels, commonly associated with thrombi. This lesion can be easily confused with a variety of vascular lesions both benign and malignant, most importantly angiosarcoma. Although surgical excision is the mainstay of treatment, knowledge of their existence as well as meticulous preoperative evaluation are needed to avoid unnecessarily aggressive treatment of this benign lesion. We report an uncommon case of IPEH within the left submandibular region in a 56-year-old male and discuss the pathogenesis, clinical features, differential diagnosis and management of this lesion, in the light of a case report and a review of the literature.
Introduction:
Intravascular Papillary Endothelial Hyperplasia (IPEH), also called Masson’s tumor or vegetant intravascular hemangioendothelioma, is an unusual, non-neoplastic vascular lesion, characterized histologically by extensive proliferation of endothelial cells and papillary formation in normal blood vessels or vascular malformations associated with thrombi [1,2,3].
Although IPEH occurs most frequently in the skin and subcutaneous tissues of the head, neck, trunk, and extremities, cases manifesting as a submandibular mass are unusual [2,4].
Here, we report a case of IPEH in the left submandibular region and discuss the pathogenesis, clinical features, differential diagnosis and management of this lesion, in the light of a case report and a review of the literature.
Case Presentation:
A 56-year-old man presented with an isolated swelling in the left submandibular region, growing over a period of six months. There was no history of fever, dyspnea, dysphagia, dysphonia, recent infection or weight loss. He was a nonsmoker and reported no record of previous trauma or surgical intervention.
On physical examination, the patient was in good general health with a firm, nontender, left submandibular swelling with a long axis of 8 cm that was mobile in all directions. The overlying skin was healthy, and no motor nerve deficiency or other abnormalities were detected during the oral cavity, oropharynx and larynx examination. Clinically, it was thought to be submandibular gland neoplasm or lymphadenopathy.
Computed Tomography (CT) of the neck showed a well-circumscribed, oval hypervascular mass, measuring 65x62x78 mm in the left submandibular space with intralesional vascular enhancement (Fig 1). The lesion was clearly separate from the submandibular gland and no lymphadenopathy was detected. Fine-Needle Aspiration Cytology (FNAC) of the lesion was inconclusive and routine blood tests were normal.
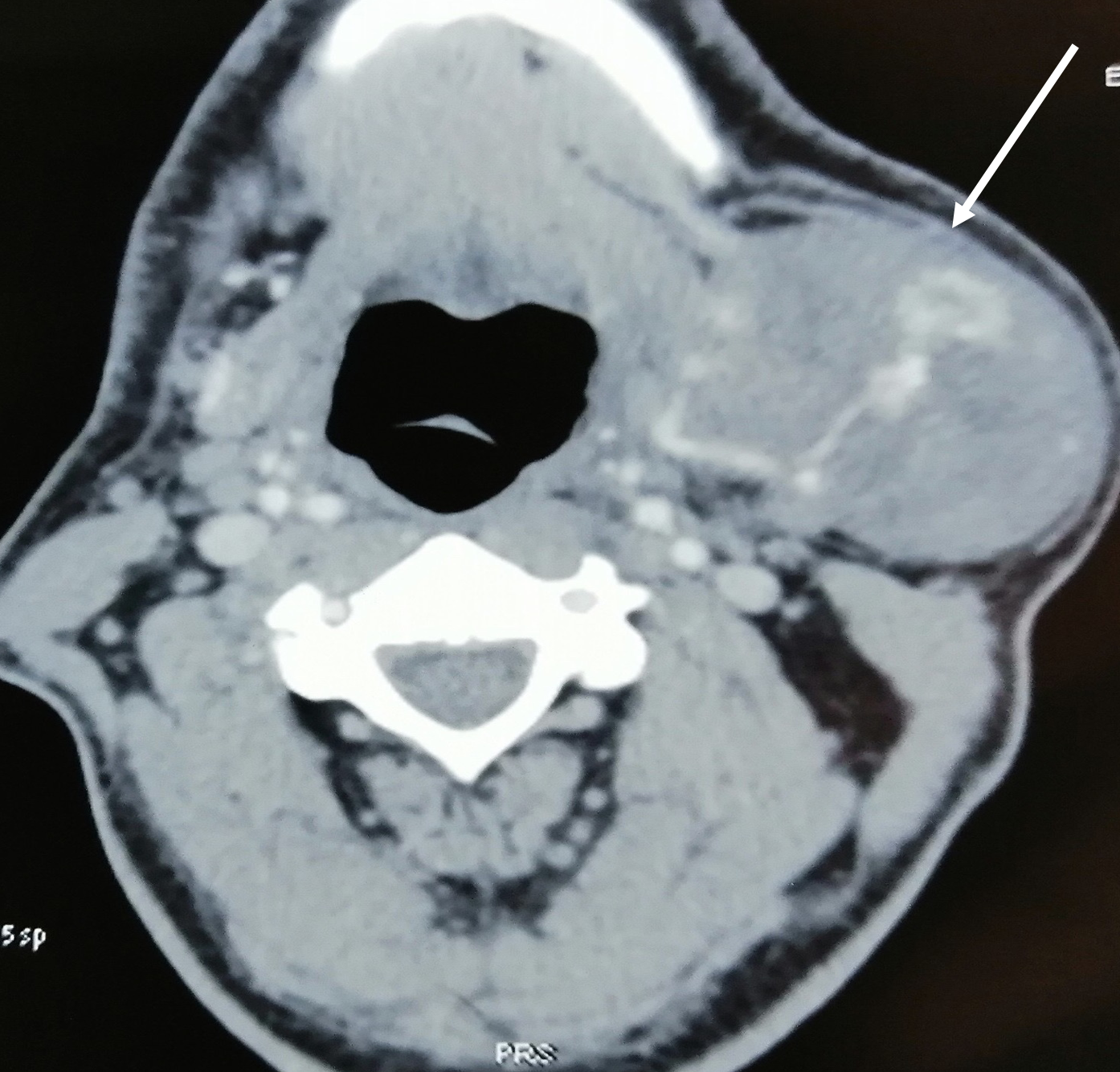
Figure 1: CT-axial scan demonstrates a well-circumscribed large heterogeneous vascular mass with dilated vessels occupying left submandibular region (white arrow)
Surgical resection under general anesthesia for definitive diagnosis and treatment was planned. A neck incision was performed to expose the left submandibular region. Intraoperatively, the tumor was well encapsulated, hypervascular with multiple feeding blood vessels and adhered to submandibular gland and base of body of mandible. The mass was dissected carefully from surrounding tissue and completely excised with feeding vessels ligation. The histopathological analysis was consistent with the diagnosis of IPEH /Masson’s tumor (Fig 2).The postoperative course was uneventful and no recurrence has been observed follow-up of one year.
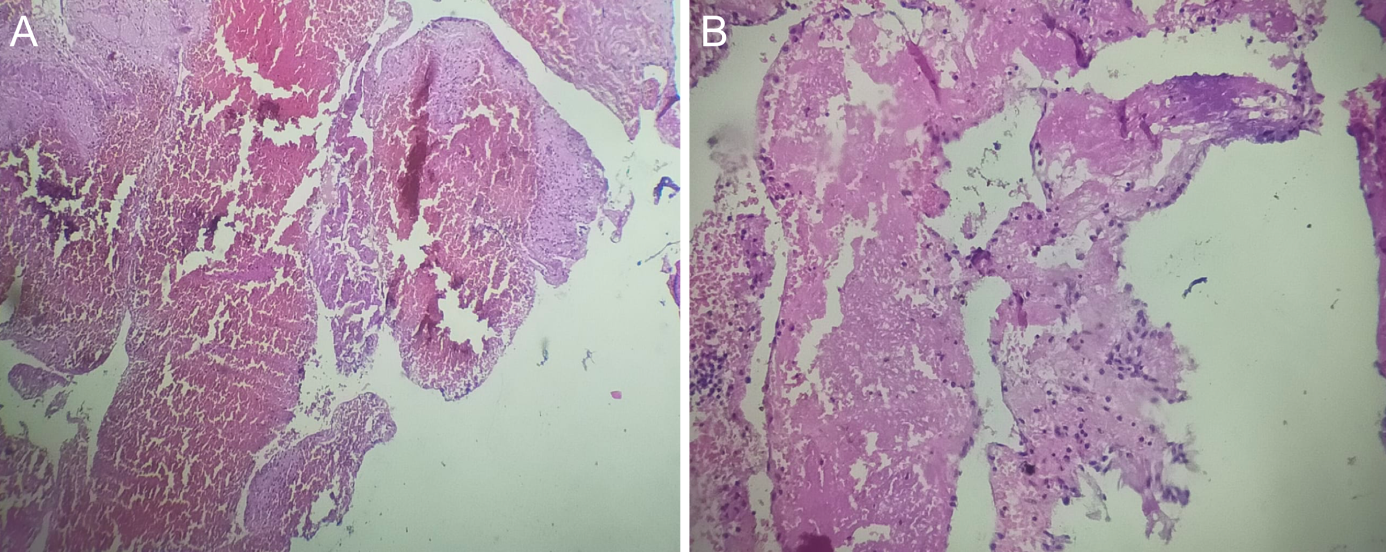
Figure 2: Histological features of IPEH, showing:
• A: Intraluminal papillary projections with a hyalinized fibrinous axis (H&E, x100).
• B: Papillae with central collagenized cores lined by a single layer of endothelial cells without cytologic atypia, mitosis or necrosis. (H&E, X200).
Discussion:
IPEH is a rare vascular tumor initially described by the French pathologist Masson in 1923 in inflamed hemorrhoidal plexus of a 68-year-old patient [1]. It accounts for approximately up to2% of benign and malignant vascular tumors of the skin and subcutaneous tissue and shows a slight female preponderance after the fifth decade of life with no race predilection [2, 3].
The pathogenesis of IPEH continues to remain unclear; some researchers believe that it is a benign neoplastic process involving endothelial cell proliferation and papillary formation within vascular lumen which undergoes degeneration and necrosis. The other possible mechanism is an unusual form of organization of a thrombus with associated perivascular inflammation secondary to trauma [2, 3]. However, three types have been distinguished [3].
IPEH can occur anywhere in the body, but it is more common in the fingers, head, neck, trunk, and extremities in the order of decreasing frequency [4, 5]. The presentation of this tumor in the form of a submandibular mass is very rare. Based on our current knowledge, only 2 case reports concerning this location have been published in the English literature [5, 6].
Clinically, it usually presents as a slow-growing mass that may be somewhat painful and imparts a reddish-blue color to the overlying skin. Thus, it can be confused with other benign neoplasms or vascular malformations [6].
Medical imaging provides a considerable contribution not only to further characterize a suspected vascular lesion,which allows its distinction from other soft-tissue masses, but also to assist the surgeon regarding the risk of uncontrollable intraoperative bleeding. Nonetheless, it is insufficient to diagnose IPEH, which requires histological confirmation [7]. Computed tomography generally shows peripheral enhancement with central heterogeneity. On MRI, IPEH produces a heterogeneous signal postcontrast, with patchy central enhancement [2,4,8].
The definitive diagnosis is based on histology during biopsy or examination of the resection specimen. However, IPEH may be histopathologically mistaken for an angiosarcoma. The IPEH is described as a well-circumscribed lesion with papillary proliferation of endothelial cells forming vascular channels, commonly associated with thrombus. There is no tissue necrosis, invasive behavior, cellular atypia or mitosis. Conversely, angiosarcoma usually exhibits an invasive growth, vascular infiltration, cellular pleomorphism, frequent mitoses and necrotic foci. [2,4,9].
Other differential diagnoses include hemangioma, Kaposi's sarcoma, spindle-cell hemangioendothelioma, malignant papillary angioendothelioma, intravenous pyogenic granulomaand intravascular endothelioma [4,5,7].
Complete surgical resection with healthy margins remains the mainstay of therapy for IPEH [2-7]. The prognosis is excellent, with a low recurrence rate [3,4]. There are no cases of malignant transformation in all reported cases. Our case is unusual due to its singular clinical presentation, namely a large Masson's tumor in the submandibular region.
Conclusion:
Although commonly presented in the head and neck region, the IPEH occurrence in the submandibular space is extremely rare. It should be considered in the histopathological differential diagnosis of angiosarcoma. Surgical management remains the mainstay of therapy for these tumors; however, the authors believe that knowledge of their existence as well as meticulous preoperative evaluation is needed to avoid overtreatment of this benign lesion. The prognosis is excellent, with extremely low recurrence rate after complete surgical resection.
Consent:
Informed consent was obtained from all participants included in the study.
Conflict of Interest:
The authors declared no conflict of interest.