Shashi Pantula, Sheldon Moniz, Hannah Seymour
Department of Orthopaedics, Fiona Stanley Hospital, Perth, Australian
*Corresponding Author: Sheldon Moniz, Department of Orthopaedics, Fiona Stanley Hospital, Perth.
Received date: February 10, 2021
Accepted date: February 22, 2021
Published date: February 23, 2021
Citation: Pantula S, Moniz S, Seymour H. “Biochemical Markers as Predictors of Mortality in Hip Fractures’’. J Orthopaedic Research and Surgery, 1(1); DOI: http;//doi.org/03.2021/1.1006.
Copyright: © 2021 Sheldon Moniz. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background:
Neck of femur fractures have been correlated with significant morbidity and mortality in the elderly population (Age >65). Predictors of mortality would provide a foundation for optimising management and stratifying high risk patients. Preoperative biochemical markers have showed promising evidence as predictors of mortality in elderly individuals sustaining neck of femur fractures.
Methods:
Retrospective cohort study of 547 patient’s over 65 years who sustained neck of femur fracture. Analysis of preoperative biochemical markers included albumin, sodium, bicarbonate, lactate, base excess, white cell count, creatinine & eGFR. These were compared between deceased (n =273) and a matched survivor (n = 274) groups at 120 days post-surgical intervention for neck of femur fractures for consecutive cases at a major tertiarycenter.
Results:
Mean ages were similar across both groups, deceased cohort; 86 years versus survivor group 83 years. Biochemical markers that were not statistically significant included lactate (P=0.33), base excess (P=0.56), bicarbonate (P=0.88) & white cell count (P=0.07). Markers that were statistically significant were sodium (P=0.04), creatinine (P<0.01), eGFR (P<0.01) & albumin (P<0.01). Creatinine was the only marker showing clinical significance, with mean levels being elevated at 110 in the deceased cohort versus 81 in the survivor group.
Conclusion:
Biochemical markers have a role in identifying patients at increased risk of mortality following neck of femur fractures with creatinine a predictor of survival rate at the 120-day post-operative mark.
Introduction
In Australia the older population has been increasing exponentially, where this cohort composed 9% of the population in 1977 increasing to 15% in 2017 [1]. Given this we are presented with larger numbers of elderly trauma patients that present with a multitude of management challenges.
Neck of femur fractures has been associated with significant morbidity and mortality, particularly within the older patient often signifying a sentinel event. The most common associated mechanism of injury is due to minor falls from minimal trauma falls accounting for 36% of cases [2]. Australian Institution of Health & welfare reports 91% cases are aged over 65 years with 40% aged over 80 years [1]. Within this 98% of deaths seen were individuals aged over 65 years [2]. Incidence is more prevalent in women with men consistently having higher death rates up to 1.7 times higher [2]. In this cohort, individuals that sustained hip fractures were 3.5 times more likely to die within a year of surgery compared to those not having a fracture [3]. Predictors of mortality risk would therefore provide foundation for optimising management in this demographic.
Biochemical markers have been proposed as tools that may be beneficial in predicting mortality. Albumin has been linked to malnutrition & frailty assessment particularly in the trauma setting [4]. Lactate levels and metabolic acidosis markers have also been postulated as predictors for mortality [5,6]. Several studies have shown promising evidence with optimisation of preoperative biochemical markers including albumin, lactate and base excess leading to reduced mortality risks in elderly trauma patients [7,8]. However, there is limited evidence with conflicting ideas requiring further exploration. The purpose of this study was to review and compare pre-operative biochemical markers in patients who suffered mortality within 120 days of surgery for neck of femur fracture that could be optimised.
Methods & Materials
We conducted a retrospective cohort study of data collected from a single tertiary centre trauma registry during January 2015 to June 2019. We identified all patients that met the following criteria:
1. Age >65
2. Neck of femur fracture between January 2015 & June 2019
3. Underwent surgical intervention
4. Mortality within 120 days of surgery
The study center has a dedicated orthogeriatric service with overall low mortality of 7% at 30 days for hip fractures with short times to surgery with minimal delays even in patients with comorbidities.
Exclusion criteria included individuals that were palliated & never attended surgery for femoral fracture.
This yielded 273 patients meeting inclusion criteria. For comparative assessment 274 patients that survived were randomized using computer generated selection with the same criteria during this time frame. Overall, 547 patient’s pre-operative markers were reviewed.
Outcome Measures
Primary outcome measure was whether admission biochemical markers were associated with mortality in patients sustaining neck of femur. For each patient age, gender and preoperative biochemical markers (including white cell count, sodium, creatinine, eGFR, albumin, lactate, base excess levels) were extracted.
Statistical Analysis
A priori power calculation was performed based on previous similar studies generating a sample size of 200 patients per group to detect a significant difference, with a power of 0.80 and an alpha of 0.05. Statistical analyses comprised of a chi-square test for categorical variables and an independent samples t-test for continuous variables performed using SPSS V24.0 (IBM Pty Ltd); significance was set at p<0.05.
Results
Review of the study population noted mean ages were relatively similar across both groups; deceased cohort was 86 years compared with 83 years in the survivor group (Figure 1). Within deceased group there was 1.5 times more females (169) then males (106). Within the survivor group there were 3 times more females (208) then males (66), however this cohort was random selected from a larger scale of patients.
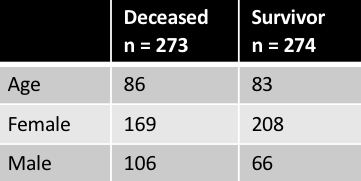
Figure 1: Demographics
Reviewing preoperative biochemical markers; lactate (P=0.33), base excess (P=0.56), bicarbonate (P=0.88) & white cell count (P=0.07) were not shown to be statistically significant and had little clinical difference between the mean levels of the survivor & deceased groups (Figure 2). In respect to lactate and bass excess levels all patients did not routinely have these values done pre-operatively therefore data sets were not complete.
Biochemical markers that did show a statistically significant difference between the deceased & survivor groups were sodium (P=0.04), creatinine (P<0.01), eGFR (P<0.01) & albumin (P<0.01) (Figure 3). However, creatinine was the only marker showing a clinically significant difference with mean levels being elevated at 110 in the deceased cohort versus 81 in the survivor group (Figure 3).
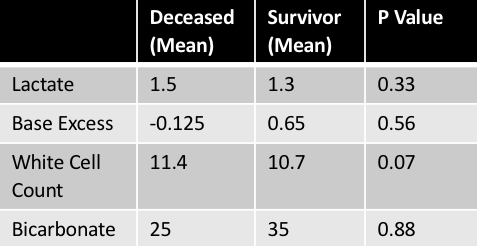
Figure 2: Non-Statistically Significant Markers
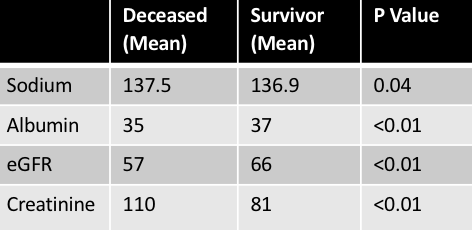
Figure 3: Statistically Significant Markers
Discussion
Physiological differences, comorbidities & polypharmacy in the elderly can result in significant alterations in response to trauma and increase risk of mortality [9]. This study aimed to investigate the predictive value of biochemical markers for mortality in elderly patients after neck of femur fractures. This was in view that optimisation may result in better patient clinical outcomes. Previous studies have noted several biochemical markers that may be beneficial as predictors of mortality. Harrison et al reviewed the utility of isolated albumin as a predictor of mortality in elderly patients with neck of femur fractures. Given albumin has been associated with indication of nutritional status and chronic illness states it can be a useful preoperative marker [10]. They noted statistically significant linked between mortality drop in albumin, stating reduction of 1g/dl in preoperative albumin was associated with an increasing mortality of 4.3% within first 12 months [10]. In our study however, we found although albumin was a statistically significant marker, clinically there was minimal differences between deceased group (35g/dl) & survivor group (37g/dl) mean.
Further study conducted by Callaway et al analysed links between lactate and base deficit levels on admission as predictors of mortality risks in elderly blunt trauma patients. This six year study showed that these markers, known to reflect occult hypoperfusion did correlate with increased mortality. Compared with the normal lactate group, patients in the severely elevated lactate group had 4.2 times higher mortality rates [4]. Higher risks were also noted between the normal base deficit groups versus severe group, with 4.1 times higher mortality rates [4]. In our study these markers were not statistically significant (p-values of 0.33 & 0.56 respectively). However, our data sets were incomplete as patients did not routinely have these tests done pre-operatively. This raises the point that if they were taken prior to surgery it was likely secondary to clinical concerns and therefore may be reflective of comorbid issues.
A meta-analysis of 15 observational studies done by Lauland et al reviewed several biochemical markers including albumin, creatinine, total lymphocyte count, haemoglobin & parathyroid hormone in patients over 60 with hip fractures. Results showed that markers that had mortality prognostic value were low haemoglobin, low total lymphocyte count, low albumin, high creatinine & parathyroid hormone [11]. Our study did also reflect that albumin, creatinine & eGFR had statistical significance however when direct comparison of the mean values between groups were made only creatinine showed clinical significance. The deceased group means were elevated at 110 compared with 81 in the survivor group. This is suggestive that potentially optimisation where possible of creatinine levels may be linked to reduced mortality risks.
Sodium, white cell count & bicarbonate levels link to mortality with hip fractures has not previously been directly analysed prior to our study. We found that with white cell count & bicarbonate they did not yield any statistical or clinical associations with mortality, however sodium interestingly was found to be statistically significant. However, at review of the mean values between the deceased and survivor groups (137.5 & 136.5 respectively) there were no real clinical differences that could potentially suggest merit in optimisation.
Limitations
Our study was a retrospective study therefore lends the potential for selection bias. Our deceased study cohort was also only focused at individuals that were deceased within the 120-day post-surgical mark. This was due to these patients having the most complete data set in the registry. Predictive value of biochemical markers may be more significant in long term mortality risk as noted in other similar studies if patients deceased at one or two years post-surgical mark were included in study. Given the retrospective nature of the study, lactate and base excess values were not able to be analysed in all patients and therefore would be better included in prospective studies that would allow all patients to have the preoperative markers requested. Finally, while we can make assumptions based on the values of theses biochemical markers we can not exclude additional concurrent physiological processes and metabolic stress that can also influence these levels.
Conclusion
Identification of suboptimal biochemical markers and optimisation may have a role in identifying at risk patients in the elderly neck of femur cohort. Particularly optimisation of creatinine levels pre-operatively potentially has a role in reducing risks of mortality. However, these markers lack sensitivity as predictors of survival rate at the 120-day post-operative mark. This study confirms that metabolic markers being deranged is not a good predictor of overall mortality and preoperative optimisation is difficult and delaying surgery for optimisation may not be warranted in this patient cohort.