
Seema Mishra1*, Raghav Gupta2, Swagata Biswas 2
1Department of Onco-Anaesthesia &Palliative medicine, Dr. BR Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, Delhi, India
2DM Onco -Anaesthesia Resident, Department of Onco-Anaesthesia &Palliative medicine, Dr. BR Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, Delhi, India
*Corresponding Author: Seema Mishra, Department of Onco-Anaesthesia &Palliative medicine, Dr. BR Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, Delhi, India.
Received: April 20, 2021
Accepted: April 30, 2021
Published: May 10, 2021
Citation: Seema Mishra, Raghav Gupta, and Swagata Biswas. (2021) Challenges encountered by palliative care physicians in the cancer care setup in India during novel COVID 19 pandemic, J Oncology and Cancer Screening, 2(4); DOI: http;//doi.org/04.2021/1.1020.
Copyright: © 2021 Seema Mishra. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
COVID 19 pandemic by its sheer magnitude has posed enormous amount of burden on healthcare facilities across the world, with its maximum impact being borne by resource limited settings. Also, the patients suffering from immunocompromised state like cancer are getting afflicted the most by the infection. But at the same point of time concerns of pain and palliative care physicians working in cancer care setups should not be overlooked as they are facing many challenges on various fronts like at the level of infrastructure, personal or at the level of non-governmental based palliative care services. To overcome these challenges, it is important first of all to identify these challenges in various setups across the country, as these challenges may differ between different cancer care setups. Once the identification is done then it becomes imperative to address these challenges and concerns of the physicians and on the basis of which health care facilities, government and private sector organizations should come together and mitigate these challenges of pain and palliative care physicians so that they can provide their best services to all the patients in need with full conviction and enthusiasm.
Introduction:
The COVID‑19 pandemic hit most healthcare providers globally in a way they did not anticipate. It has also resulted in economic, social, and political devastation rapidly becoming an international public health crisis [1]. The WHO declared the disease as pandemic on 12th March 2020 and urged countries to limit its spread [2]. In India also the count is rising steadily, experts believe that India is currently in the stage of limited community transmission, which is expected to progress over the next few weeks. The older patients and those with underlying serious health conditions for example cancer, have an increased risk of admissions into intensive care units [3, 4]. The estimated case fatality rate in cancer patients with COVID‑19 is 6% [5], as compared to 1% among the general population [6]. With the estimated number of cancer cases in India being approximately 2.25 million the impact of this pandemic on cancer patients will be grave affecting both survival as well as quality of life [7]. Palliative care with its holistic approach, motto of giving realistic hope and honest opinion, focus on symptom management (physical, psychological, social and spiritual), expertise in discussing prognostic uncertainty, establishing goals of care based on patient and family values and preferences, and support of the caregivers and families provides an option for taking care of cancer patients suffering with pain [8,9]. Policies of social distancing, staff shortages and announcement of nationwide lockdown on 25th March 2020 to mitigate the spread of novel COVID 19 pandemic have impeded the ability of pain and palliative care physicians to provide quality care. Thus, it is imperative to formulate a standard operating protocol so that uninterrupted and good Pain and Palliative care services can be provided to all the cancer patients. In this review article, we highlight and discuss the barriers and challenges encountered by physicians working in cancer care setup at various levels so that on the basis of which solutions could be formulated.
Role of Palliative care services during COVID 19 pandemic:
COVID 19 pandemic has come as a bane for the society, especially from two aspects- one for the countries and setting with limited health care infrastructure and resources and other for the patients suffering from debilitating illness like cancer who are already immunosuppressed and come under high-risk category for contracting SARS-CoV-2 infection [4]. The brunt of the whole process is being faced not just by the patients and their caregivers but also by the health care providers who are facing multiple challenges and hurdles on various fronts. Pain and palliative care physicians have a very important role to play during this COVID 19 pandemic especially for cancer patients whose treatments have been deferred but are suffering in lot of pain due to disease progression. They can also coordinate with other primary disciplines managing oncology patients in a comprehensive manner and chart out a proper care plan [10].
Challenges for the pain and palliative care physicians:
All the pain and palliative care physicians throughout the country have been working day in and day out since the onset of this pandemic with full dedication to provide their best services so that the cancer patients suffering from various symptoms are well managed. Less than 1% of population has access to pain relief and palliative care [11]. But during the whole process of catering to patients they themselves have to encounter hurdles and challenges at various levels. Following are the details of challenges at various levels faced by physicians
1.Challenges at the level of infrastructure and hospital:
All the healthcare facilities have curtailed their registrations be it for inpatients or outpatients. This has been done keeping in mind the norms of social distancing and to prevent overcrowding in the hospitals. These policies become even more relevant in oncology setups because cancer patients are immunocompromised and can easily contract infections [4]. Because of these new regulations all the health care workers face the ethical dilemma because they now need to triage the patients based upon their severity of signs and symptoms into three groups e.g., high priority group (require in hospital palliative care), medium priority group (require in hospital palliative care after failure of home-based management) and low priority group (home based palliative care) [12,13]. Thus, physicians cannot cater to all the patients and care givers coming to hospitals like before COVID 19 pandemic [14]. It has been reported by Kumar that there are approximately 1000 palliative care units in India, with about 90% of these being located in Kerala [15]. The problem gets compounded by the restricted entry to the number of caregivers allowed in the hospital premises, so now physicians cannot provide them with well needed psychosocial support to all the family members which is a very important aspect of cancer care. This not only leads to dissatisfaction amongst the patients and caregivers but also takes a toll on emotional wellbeing of the physicians, as they feel that they have not been able to dispense their professional duties for all the patients equally. Role of allied health services like physiotherapy, wound care services form an important component of whole treatment process of cancer patients, but access to all these facilities have also come down drastically during the pandemic. Advanced cancer patients are in need of essential medications like opioid most of the time to manage their pain [16], but due to logistic challenge of transportation during lockdown they were not able to procure their pain medications as these are available only at few tertiary cancer care centers in the country. Most of the other hospitals nearby their home do not have pharmacy dispensing wings which can provide them with these essential medications. To overcome the challenge of curtailed outpatient facility many centers advocate for the use of telemedicine facility so that the patients can be provided with online consultations for their minor symptoms so that they don’t need to travel all the way to the hospital. But still many places because of limited resources available with them are not able to provide patients with teleconsultations, eventually leading to increased suffering for cancer patients and their caregivers. Because of the resource limited settings there is inadequate amount of place in many health care infrastructures to adequately screen the patients for COVID-19; also, the testing facilities are limited even if the patient is a COVID suspect. Eventually because of limited testing and screening facility there is always a possibility of attending a COVID positive patient in the pain and palliative care outpatient department, posing a significant amount of risk for all the healthcare workers. On the academic front, also one of the hurdles faced by physicians is that that research pertaining to pain and palliative care has been afflicted as the focus has been shifted towards research pertaining to COVID. To overcome these challenges faced by physicians we suggest few solutions so that if ever encounter such pandemic or catastrophe in the future we are fully prepared to face that. The public health infrastructure has to be revamped and more allocation of the gross domestic product of the country should be towards the health industry. It should not be contemplated as an expense but rather as an investment for the future. There should be an increased use of technology in the healthcare facility and use of telemedicine should be encouraged whenever and wherever deemed suitable. Separate task forces should be formed by hospitals to deal with separate aspects with special emphasis on specialist palliative care services in every hospital. Educational and training sessions should be conducted on regular basis for all health care providers so that they are updated with latest research and development in the field of medicine. Standard operating protocols should be developed by individual hospitals and national level guidelines should also be formulated so that they can be followed by all health care professionals. Essential medications and equipments should be stockpiled by the hospitals so that patients don’t have to run every nook and corner to get pain relief which is a humane right for every patient. Communication is one of the most important pillars on which the whole efficacy of treatment process relies upon, so advanced care planning should be practiced for the cancer patients coming to the hospital. This will instill confidence in the patient as well as family members. (Table 1)
|
Challenges |
Solutions |
|
|
Table 1: Challenges at the “Level of infrastructure and hospital”
2.Challenges at personal level of physicians:
Challenges faced by pain and palliative care physicians in cancer care setup has not been just at the hospital level but also at the personal front also. During the time of nationwide lockdown there has been a huge problem regarding the commutation to the workplace as the public transport facilities are curtailed. The whole pandemic saga has created a huge panic and anxiety amongst the healthcare professionals also as they have a fear of contracting infection from the workplace. Moreover, there is a sense of fear that they may carry the infection back home and transmit to the small kids or elderly members in the family. Many health care workers who are posted at dedicated COVID facilities have to remain away from their families for a prolonged period of time which in itself leads to depression. Those health care professionals living in the rented accommodation are always afraid that they may face discrimination from the society and maybe asked to vacate from their accommodation. In the hospitals, the biggest hurdle faced is difficulty in communicating and convincing the cancer patients and their caregivers regarding reasons of shift in goals of cancer treatment. Cancer patients are worried about their cancer progression because of delay in anticancer treatment (surgeries, chemotherapy and radiotherapy sessions). This has led rapidly increase in anxiety levels in cancer patients. With many health care professionals also getting afflicted by the corona virus infection the workforce decreases, so the onus of the clinical work shifts onto the remaining staff. This leads to long working hours leading to burnout amongst the physicians. The biggest armamentarium for the health care worker during this COVID-19 pandemic is personal protective equipments (PPE), but inadequate supply or poor quality of PPE decreases the morale of all the physicians. Also, because there is inadequate training regarding the pain and palliative care at the grassroots level, the onus of handling palliative consultations falls on a very limited number of physicians. Another challenge faced at the personal level on the academic front is to keep oneself abreast with the latest literature and guidelines coming up on daily basis related to COVID. Keeping in mind all these challenges at personal level there can be few solutions which can be utilized to mitigate them. Till the time public transport facilities are not fully restored, hospitals should try to reach out to government and try to provide the transport facilities for its workers round the clock, as they are the backbone of the infrastructure and their comfort to reach their workplace is imperative. Regular counseling and meditation sessions should be conducted for all the physicians so that they are able to relax themselves in this stressful environment. All the physicians should be divided in different COVID and Non COVID pools. All should not be called simultaneously to the workplace; there should always be a reserve workforce available in case someone gets infected then the rest of the team members can take over their clinical work. Judiciary should form stringent laws for the people involved in creating social discrimination. Government should make an effort to create awareness in the public regarding important role played by the doctors as frontline warriors at this point of time and there should be no social discrimination against them. Production of PPE should be ramped up and it should be ensured by the government that there should be uninterrupted supply of good quality PPE for all the physicians. (Table 2)
|
Challenges |
Solutions |
|
|
Table 2: Challenges at “Personal Level”
3.Challenges at the level of home and hospice-based pain and palliative care services:
In the field of oncology there are numerous non-governmental organizations and hospices working for the welfare of cancer patients who cannot travel all the way to hospital in their terminal stages or cannot afford the hospital expenses. But this era of COVID pandemic has hampered the services provided by these organizations also. They are providing the patients with limited services because of lack of their support staff, inability to go to patients’ home and limited availability of PPE with them. So, the help the pain and palliative care physicians were able to avail from them has also decreased drastically. The number of admissions done by hospice services has also decreased in a spiral fashion. (Table 3)
|
Challenges |
Solutions |
|
|
Table 3: Challenges at the “Level of home and hospice-based pain and palliative care services”
Adaptation strategies to overcome the challenges faced during COVID pandemic:
There can be various methods and strategies to mitigate the effect of this global pandemic on providing pain and palliative care services for cancer patients. We propose few of these strategies with the acronym PALLAITE for palliating the COVID 19 pandemic. (Table 4).
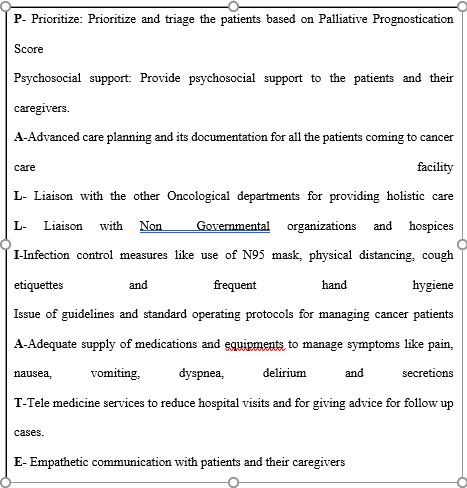
Table 4: PALLIATE Strategy: For Palliating the COVID 19 Pandemic
Conclusion:
COVID-19 pandemic has jolted the healthcare system of entire world be it in developed nation or developing nation like India. The consequences of the infection in terms of mortality have been maximum in immune-compromised patients suffering from diseases like cancer. This burden has to be borne by both patients and their physicians alike. The pain and palliative care services have hit a roadblock because of the challenges encountered by the physicians at various levels like at the level of infrastructure, personal or at the level of non-governmental based palliative care services. To overcome these challenges it is important first of all to identify these challenges in various setups across the country, as these challenges may differ between different cancer care setups, once the identification is done then it becomes imperative to address these challenges and concerns of the physicians and on the basis of which health care facilities, government and private sector organizations should come together and mitigate these challenges of pain and palliative care physicians so that they can provide their best services to all the patients in need with full conviction and enthusiasm.
Declaration of interest statement: The authors report no conflict of interest. The authors alone are responsible for the content and writing of the article