
Martynov Vladimir Leonidovich 1*, Pechilin Nikolay Nikolaevich 2
1 Doctor honey. sciences' Resident hir. otd. GBUZ BUT "city clinical hospital № 12", Nizhny Novgorod 603033, Nizhny Novgorod, ul. Zaprudnaya, d. 3, sq. 176. Honeycombs'.
2 Resident of the surgical department of GBUZ NO "GKB No. 12" in Nizhny Novgorod, Russia
*Corresponding Author: Martynov Vladimir Leonidovich , Doctor honey. sciences' Resident hir. otd. GBUZ BUT "city clinical hospital № 12", Nizhny Novgorod 603033, Nizhny Novgorod, ul. Zaprudnaya, d. 3, sq. 176. Honeycombs'
Received: April 15, 2021
Accepted: April 20, 2021
Published: April 26, 2021
Citation: Martynov Vladimir Leonidovich, Pechilin Nikolay Nikolayevich. (2021) Cag Repeats and Cancer Probabilities – Not A Hard and Fast Rule, J Oncology and Cancer Screening, 2(2); DOI: http;//doi.org/04.2021/1.1019.
Copyright: © Martynov Vladimir Leonidovich. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Violations of the microcirculation of the intestinal wall tissue along the anastomosis during the formation of the intestinal anastomosis by the ligature method are 4 times higher than those with compression methods. In emergency surgery, with an intra-abdominal pressure of the II degree and more, primary anastomosis is contraindicated due to severe microcirculation disorders in the intestinal wall due to the underlying pathology and the method of formation of the anastomosis. A new publicly available, safe inter-intestinal delayed compression anastomosis has been developed and introduced into clinical practice, eliminating many complications of the formation of the anastomosis and complex reconstructive surgery.
Introduction:
The presence of a large number of methods for the formation of inter-intestinal anastomoses, including compression, and the continuously ongoing work of surgeons in this direction, suggests that at present there is no “ideal” method for connecting intestinal loops. Nevertheless, the formation of an anastomosis is a key step in the surgery on the hollow organs of the gastrointestinal tract. However, the application of new techniques and tactical algorithms does not radically solve the problem of anastomosis.
Many researchers see the main reason for the development of this complication in peritonitis, in the conditions of which emergency resection of the intestine occurs, when significant changes occur in the intestinal wall itself. Among them, a violation of microcirculation, membrane digestion, inhibition of the active transport of glucose, synthesis of nucleic acids, enzymes of oxidative phosphorylation, an increase in the concentration of active plasmokinins, inhibition of intracellular immunotropic mechanisms. All of the above determines the inhibition of the regenerative activity of intestinal tissues, which prevents the normal healing of sutured intestinal wounds [Zaitsev E.Yu., 2009; Sheyanov S.D., 2009].
A high risk of developing local and generalized complications is directly associated with critical microcirculation disorders in the intestinal wall. It is known that one of the main causes of such disorders in the wall of the intestine is an increase in intra-abdominal and intestinal pressure, which leads to compression of the microvessels, the development of venous stasis and interstitial edema. At the same time, there is a strong direct correlation between these effects in acute intestinal obstruction. The nature of the morphological changes in the wall of the small and colon colon depends on the severity of intestinal obstruction. Increased intestinal pressure to 31 mm RT. Art. even within 30 minutes, significantly impairs the performance of intramural blood circulation of the small and colon [Lukoyanychev E.E., 2011; Ryabkov M.G., 2015].
Intraabdominal hypertension complicates acute obstruction in 30-70% of patients and leads to the development of abdominal compression syndrome in 7-10% of them. In patients with established intra-abdominal hypertension syndrome, mortality is 68% [Eddy V. et al., 1997]. These disorders manifest with increasing pressure already up to 15 mm Hg. Art. With an increase in intra-abdominal pressure up to 25 mm RT. Art. Ischemia of the intestinal wall develops, which leads to the translocation of bacteria and their toxins into the mesenteric bloodstream and lymph nodes. Grades II-III-IV intra-abdominal hypertension in the pre- and postoperative period causes a violation of microcirculation in the intestinal wall, respectively, by 20%, 40% and 50% of the norm, and a decrease in perfusion pressure by 30-40% [Kakubava M.R. 2012].
More specific data on the tactics of the surgeon, depending on the violation of microcirculation in the intestinal wall are as follows. At a distance of 30 cm proximal to the tumor, the level of microcirculation in the intestinal wall during obstructive colonic obstruction is reduced, according to laser Doppler flowmetry, by 20-30%, distal to the tumor by 10-15 cm, there is a decrease in blood supply by 5-10%; with gallstone intestinal obstruction at a distance of 30 cm proximal to the obstruction, the level of microcirculation is reduced by 20-25%, below the obstruction by 10-15 cm, there is a decrease in blood supply by 10-15%. A decrease in microcirculation in the proximal and distal edges of the resected intestine by more than 30% is dangerous for an anastomosis due to the high probability of failure (up to 19% of the colon, up to 13% of the small intestine, up to 3% of the small intestine) colostomy (up to 16%). With a decrease in microcirculation in the proximal edge of the resection to 15% and in the distal to 10%, a primary anastomosis on the left half of the colon is possible. The operation of choice is a left-sided Hartmann type hemicolectomy with a decrease in blood supply in the intestinal wall after a resection of more than 30% [Dzhadzhiev AB, 2009].
Materials and methods:
We have developed a hardware tube method for the formation of a delayed inter-intestinal compression anastomosis [RF patent No. 146199].
A device has been developed, which is a Fedorov clamp, on the branches of which two needles of metal permitted for medical use are located parallel to each other and are 50 mm long, 2.5 mm in diameter. On the needles there are tube-nozzles made of medical steel, the length equal to the length of the needle minus the length of the "sharpening" of the needle, and a diameter of 2.6 mm. Nozzles consist of two parts, the length of the majority determines the length of the anastomosis. For example, 10 mm and 40 mm, 20 mm and 30 mm, 25 mm and 25 mm. (Fig. 1.2).
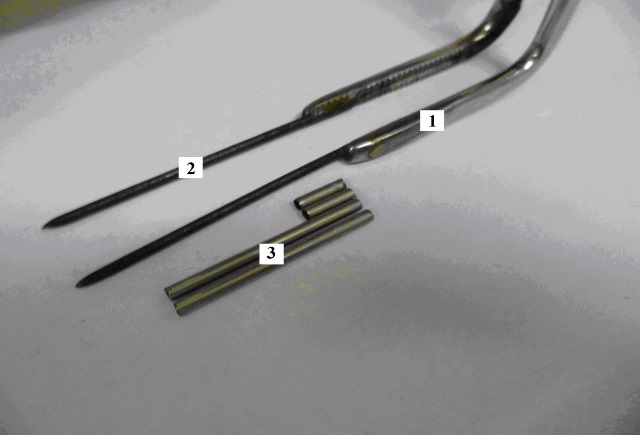
Figure 1: General view of the device:
1 - jaws of the clamp Fedorov,
2 - needles,
3 - nozzle tubes
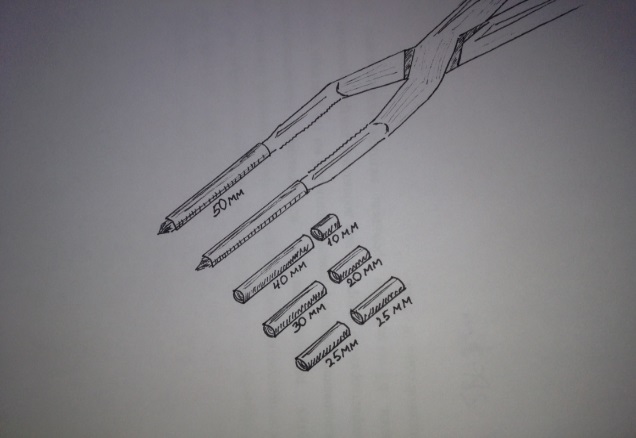
Figure 2: Sets of nozzle tubes, various in length
The device operates as follows. Tubes-nozzles are selected depending on the length of the future anastomosis and its distance from the puncture site. They put nozzles on the needles, first a smaller part, then a large part. Resection of the affected area of the intestine is performed, the distal end of the intestine is sutured tightly. The distal and proximal sections of the intestine are isoperistaltically sutured with gray-serous sutures for about 10 cm, leaving the unconnected 15 cm of the proximal section below the joint in order to further excrete it on the stoma. Departing 1 cm from the suture line, on the mesenteric collapse of two sections of the intestine, through two punctures, the device’s needles with nozzle tubes are inserted into the lumen of two sections of the intestine (Fig. 3).
The jaws of the device bring together and fix as much as possible (Fig. 4). A needle with ligatures No. 5 through the walls of the intestine is carried out under large parts of the nozzle tubes in three places (in the center and along the edges) and tightly tied, which causes constant further compression of the tissues of the walls of the two sections of the stitched intestines between the nozzle tubes (Fig. 5).
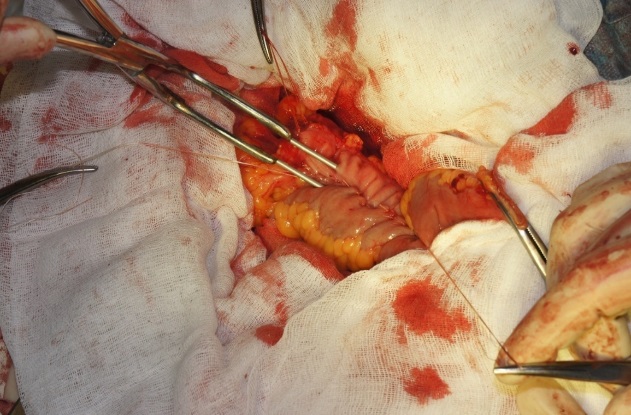
Figure 3: The establishment of needles with tubes into the lumen of two sections of the intestine
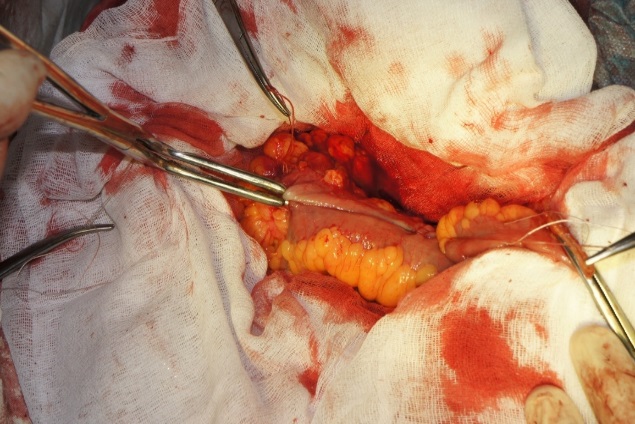
Figure 4: The device branches are as close as possible, fixed
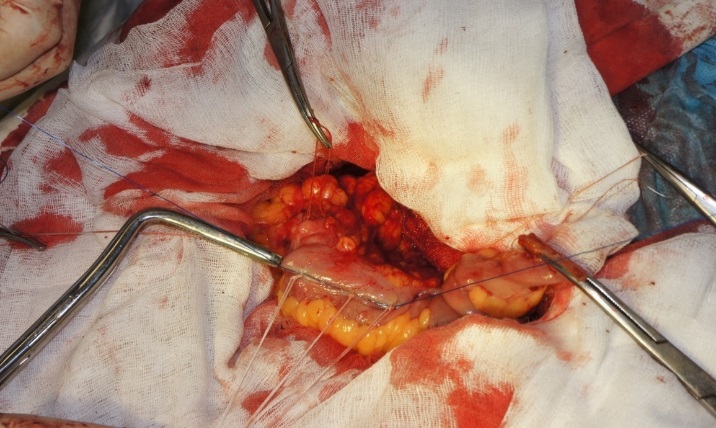
Figure 5: Three tied ligatures around the nozzle tubes
The needles with the small parts of the nozzle tubes remaining on them are removed from the intestinal lumen, leaving most of the intestinal lumen. Places of intestinal punctures are sutured with Z-shaped sutures, localizing them outside the line of the anastomosis. A second row of gray-serous sutures is applied. The proximal site is displayed on the stoma. After 8 to 11 days, necrosis of the intestinal wall tissue occurs along the compression line and the large parts of the nozzle tubes connected to each other go out into the lumen of the distal intestine, and later on with the stool out.
A similar anastomosis was formed in 38 patients aged 39 to 78 years who were operated on an emergency basis (the formation of a primary ligature anastomosis was recognized as dangerous due to intra-abdominal pressure of the II degree): in colon cancer complicated by intestinal obstruction - in 26 patients; with dolichomegasigma complicated by inversion and necrosis of the intestine - in 11 patients; with necrosis of the small intestine and diffuse fibrinous-purulent peritonitis - in 1 patient.
Results:
Normalization of intra-abdominal pressure was noted by 5-8 days, before the clinical opening of the anastomosis. Exhaustion of gases, the appearance of stool in a natural way (with X-ray evidence of the opening of the anastomosis) was noted on the 11-14th day after the operation already at normalized intra-abdominal pressure. Insolvency not noted. In the experiment, the advantage of a delayed interintestinal compression anastomosis over a ligature anastomosis is morphologically confirmed - the healing of anastomotic tissue line is in the form of primary tension.
We also found in the experiment that disturbances in microcirculation after the formation of a delayed inter-intestinal compression anastomosis are minimal. Its total indicator decreased by 9.3% and amounted to 49 pf. units (p = 0.032), and after the formation of the ligature anastomosis — by 44.4% and amounted to 30 pF. units (p = 0.032), with microcirculation = 54 pF. units (p = 0.032) intact gut.
Conclusion:
Violations of the microcirculation of the intestinal wall tissue along the anastomosis during the formation of the intestinal anastomosis by the ligature method are 4 times higher than those with compression methods. In emergency surgery, with an intra-abdominal pressure of the II degree and more, primary anastomosis is contraindicated due to severe microcirculation disorders in the intestinal wall due to the underlying pathology and the method of formation of the anastomosis
,