
Sintura V 1, Sarmukh S 1*, Azmi H 1, Prakash 2, Koay 2 , Ateeq 2, Suhaila A 3
1 Department of General Surgery, Hospital Sultan Haji Ahmad Shah, Malaysia
2 Department of Pediatric Surgery, Hospital TengkuAmpuanAfzan, Malaysia
3 Department of Pathology, Hospital TengkuAmpuanAfzan, Malaysia
*Corresponding Author: Sarmukh Singh, Department of General Surgery, Hospital Sultan Haji Ahmad Shah, Malaysia.
Received date: April 20, 2021
Accepted date: April 15, 2021
published date: May 03, 2021
Citation: Sintura V, Sarmukh S, Azmi H, Prakash, Koay, (2021) “Immature Ovarian Teratoma in Toddler. “A toddler with a balloon” A Case Report and Literature Review.”. International Surgery Case Reports, 2(3); DOI: http;//doi.org/03.2021/1.1020.
Copyright: © 2021 Sarmukh Singh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Ovarian malignancy is reported in 10-20% of all ovarian masses or neoplasm in children and comprises approximately 1% - 2% of all childhood malignancy [2]. Germ cell tumors are the most common type pediatric ovarian tumor in which ovarian teratomas are the most common germ cell neoplasm [2, 3].The incidence of immature teratoma is only1% of all ovarian cancers and 20% of malignant germ cell tumors [4].Ovarian tumor is can be life-threatening condition whose prognosis depends on early recognition, accurate diagnosis and early intervention. The age group to develop teratomacommonlyinvolve younger patients. Immature teratoma frequently occurs between the ages of 10 and 20 years, with a median age of 17 year [2]. However, in our case the age of this patient was three years old which is a uncommon cause of abdominal masses in this age group to develop teratoma. This report describes an unusual case of 3 years old child who presented with abdominal mass and was diagnosed with left ovarian teratoma and underwent exploratory laparotomy with excision of left ovarian mass
Introduction
Ovarian tumor is rare in children and the incidence increases with age. The incidence in patient 1 year of age is 0.43 in 100,000 cases and increases to 152 in 100,000 cases in 35 year old patient [1].Ovarian malignancy is reported in 10-20% of all ovarian masses or neoplasm in children and comprises approximately 1% - 2% of all childhood malignancy [2]. Germ cell tumors are the most common type pediatric ovarian tumor in which ovarian teratomas are the most common germ cell neoplasm [2, 3]. Mature cystic teratomas are the most common of ovarian teratomas and contain mature tissue of ectodermal, mesodermal, and endodermal where else immature cystic teratomaare composed of immature tissues derived from the three germ layers.3The incidence of immature teratoma is only1% of all ovarian cancers and 20% of malignant germ cell tumors [4].Ovarian tumor is can be life-threatening condition whose prognosis depends on early recognition, accurate diagnosis and early intervention. We would like to discuss regarding the diagnostic dilemma and anatomic peculiarity to facilitate the surgical resection. We advocate an excision of ovarian mass with a clear margin of may be better option for overall survival benefit and disease free survival of patient.
Case presentation
A 3 years old child presented to emergency department with worsening abdominal distension for 3 weeks duration associated with reduced oral intake. On examination, per abdomen was distended with mass palpable atsuprapubic up to epigastric measuring about 15cmx 10cm. We proceeded with abdomen x-ray showed a homogenous mass at pelvic region causing mass effect to the surrounding bowel but there were no bowel dilatation. Blood investigations showedanemic with low hemoglobin level of 9.8g/dLand thrombocytosis with platelet of 549 mcL. We proceeded with abdominal ultrasound showeda large heterogeneous solid cystic lesion extending from epigastric region till suprapubic.A CT abdomen was performed showed a huge heterogeneous enhanced solid cystic mass with internal calcification measuring 7.8cm x 11.7cm x 12.2cm (AP x Wt x CC), extends from the pelvis into the upper abdomen. The Presence of intralesional fat density, coarse calcifications with a mixed solid and cystic appearance suggestive of immature ovarian teratoma (Figure 1 and 2) [7].Tumor marker showed Alpha-fetoproteinwas raised, but Beta-HCG was normal. The child underwent exploratory laparotomy with excision of left ovarian mass. The intraoperative findings showed a well circumscribed left ovarian mass measuring 11cm x 13cm with cystic and solid in nature (Figure 3 and 4). TheHistopathology showedimmature tissue derived from the ectoderm, mesoderm, and endoderm typically mixed with mature element. Immunohistochemistry showed S100 positivity. A diagnosis of immature ovarian teratoma was made. Patient had a good speedy recovery and was discharge home. Patient was seen after 1 month at outpatient clinic and plan for monthly surveillance with serum AFP level monitoring.
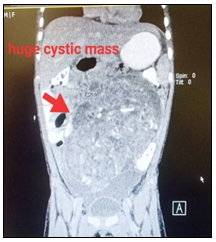
Figure 1: Showed sagittal reformatted CT scan a huge heterogeneous enhanced solid cystic mass with internal calcification is seen within the abdomen measuring approximately 7.8 cm x 11.7cm x 12.2cm (AP x Wt x CC),extends from the pelvis into the upper abdomen. Presence of intralesional fat density, coarse calcifications with a mixed solid and cystic appearance classical appearance of immature ovarian teratoma
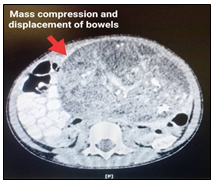
Figure 2: Showed Axial reformatted CT scan of compression and displacement of the adjacent bowels superoposteriorly and urinary bladder inferiorly.
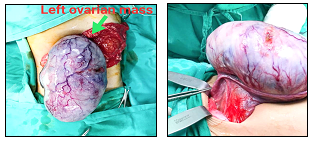
Figure 3 and 4: showed intraoperative finding of a huge well circumscribed left ovarian mass which is solid and cystic in nature.
Figure 4: Immature tissue derived from the ectoderm, mesoderm, and endoderm typically mixed with mature element. The ectoderm element composed of glial tissue, skin appendages mesodermal elements include bone, cartilage, muscle, nerve and immature mesenchyme tissue. Endoderm elements show of lung tissue and colonic tissue. Scattered neuroepithelium is seen.
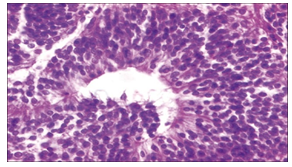
Figure 5: Immature neuroepithelium seen in the form of neuroepithelial rosettes in the immature teratoma upon histomorphological examination (Hematoxylin and Eosin stain, ×400) [9]
Discussion:
Retroperitoneal masses are the predominant abdominal masses occurring after neonatal period. In a study conducted in Rajasthan by Meena et al, 52% which is 26 out of 50 abdominal masses are retroperitoneal masses followed by hepatobiliary mass (16% of cases),
Gastrointestinal / mesenteric origin (12% of cases) and genital system only comprises of 12% of total cases [5].
Thediagnostic dilemma is the unusualpresenting symptoms which are acute or continuous abdominal pain. Besides that the mass effect to surrounding organs, such as urinary or bowel transit disorders, nausea, vomiting, increase of abdominal volume, and much rarer early puberty or vaginal bleeding [1].
The age group to develop teratomacommonlyinvolve younger patients. Immature teratoma frequently occurs between the ages of 10 and 20 years, with a median age of 17 year [2]. However, in our case the age of this patient was three years old which is a uncommon cause of abdominal masses in this age group to develop teratoma.
The first diagnostic step in young girls with suspected adnexal masses is to detect the exact site of origin and to differentiate the lesion from other disease with similar symptoms [2]. Transabdominal ultrasonography is the initial imaging modality of choice due to easily availability.On US, the appearance of the immature teratomas varied from solid to cystic. Meanwhile, the mature ovarian teratomas showedpredominantly cystic appearance with hyperechoic foci with posterior acoustic shadowing suggestive of presence of calcified components. The computed tomography (CT) should be performed to obtain additional information such as nature and extent of tumor [2]. Imaging findings also can help to predict malignancy as malignant tumor predominantly solid or heterogenous and tend to be larger than tumor. However, MR imaging is the preferred imaging modality due toit high sensitivity and specificitywith excellent soft-tissue contrast. However, the MR imaging examination requires sedation and not easily available in district hospitalin that case CT scan remains the imaging modality for the staging of ovarian tumors and for surgical planning.
Serum AFP level is elevated in patients with GCTs such as yolk sac tumors, immature teratomas, embryonal carcinomas, and mixed GCTs with yolk sac elements [2]. In our case the serum AFP was raised.Meanwhile, serum Beta-hCGis elevated inchoriocarcinoma andembryonal carcinoma. The serum CA-125 levels is commonly elevated in epithelial ovarian cancers. Soelevated AFP, b-hCG, and CA-125 levels should raise the concern for ovarian malignancy. [2]
Immature Teratomahas a more aggressive behavior and a worse prognosis compared to mature teratomaand elevated serum AFP levels have been reported in 33%–65% of patient. Immature teratoma is predominantly solid, usually unilateral and large. Histologically, itconsist of a variable amount of primitive immature embryonal tissues derived from three germ cell layers admixed with mature tissues. The tumor appears as a large heterogeneous mass with predominantly solid or mixed solid and cystic lesions in CT and MRI [2].
Surgery remains the mainstay of treatment in ovarian teratomasaccording to the experience of many pediatric surgical centers. [8] Ovarian-sparing surgery might be successfully appliedunder particular conditions. [8] Preservation of ovarian tissue should be done when there is a plane of dissection between the tumor and the normal ovary in the cases of localized mature teratoma[8].In the treatment of ovarian teratomas, the use of laparoscopic techniques has its supporters and opponents [8]. If a surgeon is experienced in minimal invasive surgery and the suspicion of malignancy is low laparoscopic approach might be adequate [8].Children’s Cancer Study Group demonstrated in their study that cyst fluid aspiration or spillage during surgery are not associated with relapse, thereby this factor, laparoscopy opponents might not have such importance for the final outcome [8]. However in the cases of large masses suspicious for malignancyand if surgical staging is requiredlaparotomy is the treatment of choices[8].Another important aspect that need to take into consideration in managing ovarian teratomas is their recurrence rate and the incidence of bilateral lesions [8]. After cystectomy the recurrent rate is reported between 3 to 13% [8].
The treatment of immature teratomascauses much more difficulties. Their possible malignant behavior requires proper risk classification. Among factors to be considered as those influencing the prognosis, staging is the next unclear one. There are studies recommending staging in all tumorssince malignant tumors and benign ones cannot be distinguished based only on intraoperative appearance. Different staging systems across the surgical centers renders evaluation of their significance difficult .The use of chemotherapyis another controversial aspect.To highlight some of them: chemotherapy or recurrence, only for malignant recurrence, in all cases of stage I grade 2 and higher or only in girls older than 15 .To the results of the studies which did not find evidence that chemotherapy had any significant therapeutic effects in pure teratomas and that it does not decrease relapses in pediatric population it remain one of the main argument. Malignant Germ Cell Tumor International Collaborative in its publications gathering data from four clinical trials suggest surgery alone for patients with stage I/II, grade 1/2 tumors and recommend conducting of a prospective trial of observation after surgery for patients with grade 2/3, stage II-IV tumors. This kind of approach might be supported by the results of Park et al. as they revealed that most stage I malignant ovarian germ cell tumor recurrences can be successfully salvaged by surgery and BEP chemotherapy without compromising the overall survival . In a study conducted by JustynaŁuczak* and MaciejBagłaj, adjuvant chemotherapy according to protocol TGM 95 was given to all girls with immature teratoma in their study group and they all responded well to the therapy but it remains questionable if these were real pure immature teratoma lesions.[8] The current treatment of choice for immature teratoma is surgery with unilateral salpingooophorectomy and staging procedure. [2]Surgery alone is the standard therapy regardless of stage (S; I-IV) or grade (G; 1–3) in paediatrics ovarian immature teratoma. [6]
4. Conclusion
Paediatric ovarian immature teratoma (IT) is a rare tumour. This study is to emphasize that immature ovarian teratoma should be considered as one of the differential diagnosis in younger female children that present with chief complain of abdominal mass. Early diagnosis and surgical intervensionof ovarian tumor in younger children is important. This is because the younger the patient the more likely that teratoma will be immature germ cell type and has more aggressive behavior and worse prognosis compared to mature teratoma.