
JC Mbonicura1*, W Irambona1, JB Bizimana2, S Manirakiza3
1University of Burundi, Kamenge Teaching hospital, Digestive and general surgery
2University of Burundi, Kamenge Teaching Hospital, Neurosurgery
3University of Burundi, Kamenge Teaching Hospital, Imagery
*Corresponding author: JC Mbonicura, 1University of Burundi, Kamenge Teaching hospital, Digestive and general surgery
Received date: April 07, 2021
Accepted date: April 15, 2021
published date: April 19, 2021
Citation: JC Mbonicura, W Irambona, JB Bizimana, S Manirakiza, (2021) “Combination of PDLSCs and Nanocomposite-fibrous Scaffold as Alveolar Ridge Preservation in Geriatric Patients before The Prostheses Insertion.”. International Surgery Case Reports, 2(3); DOI: http;//doi.org/03.2021/1.1016.
Copyright: © 2021 JC Mbonicura. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cite
Our goal was to contribute to the understanding of the obstructive jaundice pathogenesis during SARS-CoV-2 recovering period. This was a 51-year-old patient with no particular medical history, recovering from SARS-CoV-2 infection. He was recently discovered diabetic when diagnosed with SARS-CoV-2 infection. He underwent surgery for choledocoduodenostomy. The pancreatic biopsies and histological analysis was also performed. The histological analysis revealed lesions of acute pancreatitis. The early post-surgical follow-up was good. The follow-up CT-Scan performed after two weeks of surgery showed an overall normal pancreas.
Background
The novel coronavirus, SARS-CoV-2, discovered in December 2019, in Wuhan, China was initially known as responsible of severe acute viral pneumonia with Acute Respiratory Distress Syndrome. However, medical observations have founded extra-pulmonary symptoms due to SARS-CoV-2 virus [1,2]. Attention to the possibility of extra-pulmonary sequels, especially pancreatic sequels due to SARS-CoV-2 is currently lacking. We describe the case of obstructive jaundice by pancreatic compression of the lower common bile duct following SARS-CoV-2 infection.
Case Report
August 26, 2020, a Burundian 51-year-old patient, with no history of alcoholism or specific family history, at 6 months of anti-tuberculosis treatment for peritoneal tuberculosis with multiple nodes presented to the emergency department of KING FAISAL HOSPITAL (KIGALI) for polyuropolydipsic syndrome as the chef complaint. Laboratory investigations revealed diabetes with hyperglycemia at 16.6 mmol / l and HbAc1 = 12.3%. As part of routine screening, the patient was tested positive for COVID-19. Other laboratory investigations were normal. He denied dyspnea or any respiratory symptoms in the previous days.
He has been isolated in the SARS-CoV-2 Infection Management Center and has been discharged 10 days later with a twice negative RT-PCR.
In mid-September, he developed abdominal pain and vomiting. Biological investigations such as lipasemia were normal. But the MRI noted an exophytic process suspected of malignancy limiting the soft tissue of the pancreatic uncus along its posterior margin without any local compression (figure 1). However, an abdominal CT scan performed in April for her peritoneal tuberculosis noted an overall normal pancreas (Figure 2).
On October 10, 2020, the patient consults the emergency room of the BUMEREC Hospital for the same abdominal pain, this time with anorexia and jaundice. No other signs were found on physical examination than clinical jaundice without hepatomegaly.
Provisional diagnosis was an obstructive jaundice probably complicated by cholangitis. A complete blood count and liver function tests performed showed white blood cell count at 10990/mm3(N:5000-9000) with neutrophils at 9600/mm3(N :2500-75OO); alkaline phosphatase at 316U/L (N: 64- 306), γ-glutamyl transferase at 267U/L (N: 9-61), total bilirubin at 122micromols (N: <85.5) as the direct Bilirubin was 84micromols / l (N: <4.3); alanine aminotransferase at 294U / L (N<40) and aspartate aminotransferase at 112U / L (N: <31). The abdominal ultrasound showed a dilatation of the intrahepatic bile ducts and the main bile duct about of 10mm; multiple peri-pancreatic lymphadenopathies; a hypoechogenic lesion in the head of the pancreas about of 3cm and a dilatation of the pancreatic duct about of 6mm.
Considering those investigations, conclusion was a cholestasis on tumor of the head of the pancreas. The patient received Ceftriaxone, metronidazole, Trimethylphloroglucinol (Spasfon), Tramadol hydrochloride, Enoxaparin.
October 14, 2020, the patient developed pruritus. The biological control shows cholestasis syndrome and cytolysis again.
Laparotomy for biliary bypass, biopsy or resection of the pancreatic lesion was decided and performed on October 23, 2020. During laparotomy, there was jaundice generalized to all soft tissues. The pancreas was hard along its entire length. The extra and intrahepatic bile ducts were very dilated. The main bile duct was compressed by a hard and overall enlarged pancreas. However, there was no visualized tumor. A cholecystectomy and choledoco-duodenostomy were performed. Pancreatic biopsies of the head, body and tail of the pancreas were also performed. Histological analysis of the biopsies revealed lesions of acute pancreatitis.
The early postoperative follow-up was good with clinical regression of jaundice after one week. Nevertheless, postoperative collections were noted on the control abdominal CT scan (Figure 3). Laboratory check-ups such as lipasemia, amylasia and liver function tests two weeks after surgery were normal.
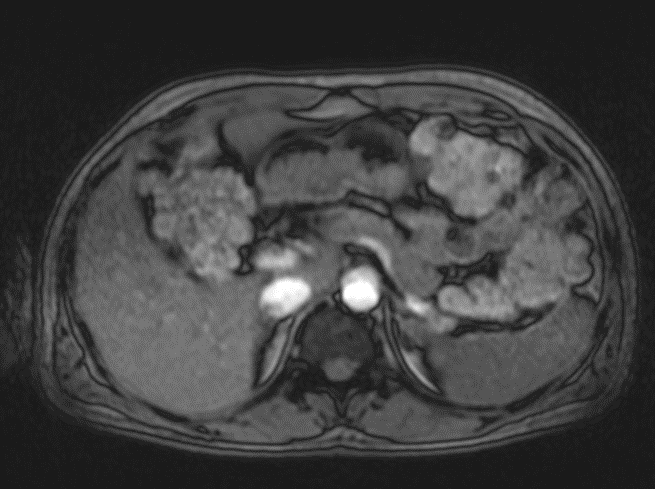
Figure 1: Abdominal MRI of September 17, 2020: exophytic process of the pancreatic uncus without any local compression.
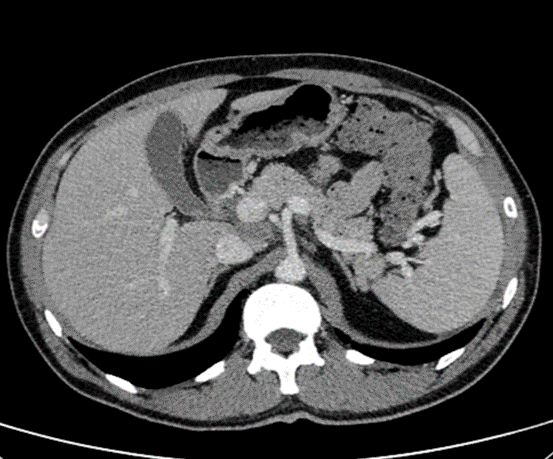
Figure 2: abdominal CT Scan: an overall normal pancreas without calcification or dilation of the pancreatic duct.

Figure 3: Abdominal CT scan: An overall normal pancreas (in yellow). But, two collections, one about of 6.7 × 4.4cm (in green) in the gallbladder region; the other about of 14 × 5.2cm (in blue) in the retro-gastric region both probably due to bilio-pancreatic surgery.
Discussion
Pancreatic damage is currently correlated to the expression of ACE2 in the pancreas where it is slightly higher expressed than in the lungs [3].
The pancreatic damages in our patient would probably be related to the sequels of the SARS-CoV-2 infection. Liu et al. [4] in a retrospective study noted structural damages such as focal enlargement of the pancreas or dilatation of the pancreatic duct without acute necrosis in 7.46% of cases in the severe form of COVID-19. Our patient only had the mild form of the disease. Pavon et al. [5] showed the possibility of direct damages from SARS-CoV-2 on different organs which accumulate with potential long-term impacts. For Dennis el at. [6], even the low-risk individuals would be exposed to a risk of organic damages affecting the heart, lungs, liver and pancreas a few months after contamination, especially when symptoms persist. Pancreatic damages would occur in 17% of cases.
Jaundice in our context would then be the result of a process of compression by an enlarged pancreas. The enlargement would probably have started during the active phase of the infection so that the jaundice clinically appeared during the recovery period of the infection.
However, cases of obstructive jaundice in pancreatic tuberculosis with histological evidence have been reported [7]. Nevertheless, in the present context, even though the patient had peritoneal tuberculosis, the pancreatic lesions appeared after 6 months of well-conducted anti-tuberculosis treatment and following his SARS-CoV-2 infection. In addition, the results of the histological analysis revealed lesions of acute pancreatitis, without any histological evidence of pancreatic tuberculosis.
No other causes of his acute pancreatitis were founded. In the literature, in addition of a few cases of acute pancreatitis reported during the acute phase of COVID-19 [8], a case of acute pancreatitis in the COVID-19 recovering period with two negative RTP-CR results was reported by Al Harmi et al. in a 52-year-old patient. No evident cause of the pancreatitis was found [9]. Furthermore, Inamdar et al. [10] note a proportion of acute idiopathic pancreatitis in COVID-19 patients up to 69% compared to the patients without COVID-19 infection.
Considering the pancreatic involvement in other coronavirus infections and the expression of ACE2 in the pancreas, this pancreatitis may be attributed to the virus [3].
Although hyperglycemia have been reported during SARS-CoV-2 infection in both diabetic and non-diabetic patients [2], HbAc1 at 12.3%, in our patient, indicates a probably pre-diabetes risk. Then, the polyuropolydipsic decompensation was possibly due to the COVID-19.
Finally, was the surgery justified? In this context, the patient presented jaundice with intense pruritus as well as cholestasis. It was therefore necessary to divert the bile for the relief of the patient and the prevention of complications. This remind us the question about specific preventing measures against COVID-19 contamination in the operating rooms.
Conclusion
Our case seems to be the first reported case of obstructive jaundice following SARS-CoV-2 infection. It seems that COVID-19 patients are at risk of developing late complications from the infection. And this for all forms of the disease. Further studies on the susceptibility of COVID-19 damage in extra-pulmonary organs (especially hepato-bilio-pancreatic) would help to understand the pathogenesis of the infection.