Demissu Afferu *, Teresa Kisi, and Yealemwork Kerie
College of Health Sciences, Department of Public Health, Arsi University, Ethiopia
*Corresponding authors: Demissu Afferu, College of Health Sciences, Department of Public Health, Arsi University, Ethiopia.
Received: April 16, 2021
Accepted: April 20, 2021
Published: May 30, 2021
Citation: Afferu D, Kisi T, Kerie Y, (2021) Determinants of treatment outcome among Tuberculosis patient in Jeju Woreda, Arsi Zone Oromia Regional state Ethiopia 2019”. International Journal of Epidemiology and Public Health Research, 1(2); DOI: http;//doi.org/03.2021/1.1008.
Copyright: © 2021 Demissu Afferu. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Successful Tuberculosis treatment out comes are the most important to control tuberculosis. Due to poor treatment out comes new strain of tuberculosis are raising and it is a serious public health concern. It is compelling to identify, and deal with factors determining treatment outcome.
Objectives:- To identify Determinants of treatment outcome among Tuberculosis patients in Jeju woreda ,Arsi zone Oromia Regional State Ethiopia 2019.
Methods:- A case control study was used where case were unsuccessfully treated and controls were successfully treated patients. Data was collected by stratified random sampling method and prepared checklist from patients taking DOT in four health centers from June 28/2009 to June 27/ 2018 in Arsi Jeju woreda.The study was done from September 4-14/2019 on 509 controls and 127 case,636 total samples. The sample size was calculated by Epinfo version7 with CI 95% , power 80% and 1:4 case to control ratio. The samples were selected from TB registration book. Bivariate and multivariate logistic regression analyses were used with 95% confidence interval. Variables with p value <0.2 in Bivariate analyses were moved to multivariate logistic regression. Variable with P value < 0.05 in multivariate analyses had significance association with TB treatment out comes.
Result: - The case group was composed of 93(73% response rate) patients with poor treatment outcome while the control group was composed of 509(100% response rate) patients with good treatment outcome. Un corrected drug dose during second phase treatment (AOR=17.949 CI 95% 3.528-91.326), decrease weight at continuation phase (AOR =10.681 CI 95% 3.076-37.098),) positive sputum result at second month and HIV co-infection were the most determinant factors for unsuccessful treatment out comes of TB patients.
Conclusion and Recommendation:-Patients with weight loss , positive smear result at second month, uncorrected drug dose at second phase of treatment and HIV positive patients were at higher risk for poor treatment out comes. While patient with increased weight, negative smear result at the end of second month, corrected drug dose at second phase of treatment and HIV negative TB patient were greater chance for good treatment out comes. Evaluation of weight and smear result at second phase of treatment and taking action for patient do not increase weight and unable to convert their smear result and HIV co-infected patients needs close follow up and corrective action would be taken for at risk patients. Corrected drug dose should be given at second phase of treatment.
1. Introduction
1.1 Background
Tuberculosis (TB) is an airborne infectious disease caused by rod-shaped acid-fast bacillus Mycobacterium tuberculosis (MTB). It typically affects the lungs (pulmonary TB) but can affect other parts of the body as well (extra pulmonary TB). TB is transmitted through droplets from an infected person with active pulmonary disease released in the air through cough, sneeze or talking and then inhaled by another person (1).
Most infections with the bacteria do not cause TB disease and 90-95% of infections remain asymptomatic (2). TB can cause infection in persons with impaired immunity (3) . Many infections do not have symptoms, known as latent TB, where in about 10% of these latent infections can develop disease in lifetime which can kill about half of those infected (4). The symptoms of active pulmonary TB disease are coughing, with sputum or blood, chest pains, fever, weight loss and night sweats.
Worldwide, TB is one of the top 10 causes of death and the second leading cause from a single infectious agent next to HIV/AIDS. In 2017, TB caused an estimated 1.3 million and 300 000 deaths among HIV-negative and positive people. Globally, the best estimate is that 10.0 million people developed TB disease in 2017: 5.8 million men, 3.2 million women and 1.0 million children. There are cases in all countries and age groups, but overall 90% are adults (aged ≥15 years), 9% are people living with HIV (72% in Africa) (5).
According to hospital statistics data, TB is the leading cause of morbidity, the third cause of hospital admission and the second cause of death in Ethiopia(6). Ethiopia is one of the countries that are highly affected by TB epidemics and ranked 7th among the 22 high TB burden countries in the world and third in Africa (6, 7)
Treatment outcome is the end health status of TB patient after taking anti TB treatment .It can be successful treatment outcome (cured +completed) or unsuccessful (died, defaulter, failure).The goal of TB treatment is not only to cure the disease ,but also to prevent its transmission and the development of drug resistance TB which is achieved by DOT of short course chemotherapy regime (8).
Tuberculosis (TB) is curable when adequate anti tubercular treatment (ATT) is properly administered. Since direct observation treatment (DOT) strategy have been initiated by WHO favorable treatment outcomes are achieved in about 85% of sputum smear-positive patients receiving standard short-course chemotherapy (9).
WHO recommend 85% of cure rate and 90% treatment success rate for well performing TB programs ,which is adequate in reducing TB transmission ,morbidity and mortality. To achieve the required treatment outcomes WHO introduce DOT (10).
1.2. Statement of the problem and Justification of the study
1.2.1. Statement of the problem
WHO set strategy for every country to reach treatment success rate ≥ 90% by 2025 (11). However, globally treatment success rate was only 83% and 82% in 2015 and 2016 which shows poor improvement(5, 12) . The overall pooled TB treatment success rate from 2005-2017 was 86% in Ethiopia which was below the WHO treatment success rate recommendation (13).TSR increase from 84% (2015) to 90%(2016) in our country (5, 12).
TB can be resistance to the drug used for treatment, when this occurs, treatment is still possible, but it is complex, long, challenging and expensive .Globally ,it is estimated that nearly one in 25 new TB case and one in five previously treated cases of multidrug resistance TB (MDR TB) (7).
Different study result in Asia and Africa shows poor/unsuccessful treatment out comes; mainly treatment failure and relapse are significantly associated with the rise of MDR TB (14-16).
Generally, unsuccessful TB treatment outcome, incomplete and in adequate treatment is the most important factors that makes difficult to control TB.
1.2.2. Justification of the study
Major contributing factors for poor treatment out comes were not clearly known in the study area. It was important to look for ways of predicting TB treatment outcomes and identifying factors that were responsible for poor treatment outcomes, which will help to identify patients that are at high risk during treatment.
Determination of the factors that are significantly associated with treatment outcomes will help to plan the possible future of TB treatment follow up and control of TB in the study area and at the country level.
Therefore this study was done to identify determinants of TB treatment outcomes in the study area.
2. Literature review
2.1. Magnitude of TB treatment out comes
WHO report show that the latest treatment outcome data for new cases show a global treatment success rate of 86%,83% and 82% in 2013,2015 and 2016 respectively . In 2018 global TB report show that treatment out come in 2016 is in eastern medateralian ( 92%) ,west pacific (91%), Africa ( 82%),Europe 97%),America(75%) and south east Asia(75%) (5).
Among 376 study participants coming from low incidence (25.5%), intermediate incidence (23.1%) and high TB incidence (51.1%) , 83.8% of patient are treated successfully and only 32.4 patients are cured. The odd for cure in patients from low incidence countries are 92% lower compared with patient from intermediate and high incidence (17).
Study conducted in 2017 in India among 1912 patient taking treatment 1648(86%), of all patients 1011(81%) of pulmonary TB ,and 700(79%) of smear positive patients have favorable outcome. (18).
In china the study done in 2018 shows the treatment success rate was 92.2% among pulmonary TB case respectively (19).
Another study in Asian country including Turkeys, Korea and Pakistan shows treatment success rate was 92.6%, 83.9% and 67.8% respectively (20-22)
In Somalia the study used a sample of 385 from 2013-2016 TB patients there were 315(81.8%) successful TB-TOs. Of successfully treated cases, 33.9% are cured and the remaining completed cases. Besides, among patients with unsuccessful treatment outcome, nearly 50% were died and the rest were treatment failures and defaulters(23).
Study conducted in 2016 in South Africa Among 495 patients with treatment outcomes reported, 80% (n=394) had successful outcomes, 11% (n=55) were lost to follow-up, 8% (n=40) died and 1% (n=6) failed treatment (24).
In Ethiopia the overall pooled TB treatment success rate from 2005-2017 is 86%. TB treatment success rate for each region showed that, Addis Ababa (93%), Oromia (84%), Amhara (86%), Southern Nations (83%), Tigray (85%) and Afar (86%) (13).
In metema hospital study conducted from 2009-2012 in 2015 shows from a total of 2970 patients 2657 (89%) were new 167(5.7%) retreatment and 146 (4.9%) are transfer cases. With respect to the treatment outcomes, 65.3% were successfully treated, 88 (3.0%) died, 107 (3.3%) defaulted, 22 (0.7%) failed and 814 (27.4%) were transferred out (25).
The study done in south omo Jinka general hospital from 2004-2014 among 2156 patients result showed that 13.1% of the cases were cured, 60.9% treatment completed, 10.2% died , 9.1% were lost to follow-up and 74% the overall treatment success (26) .
Four year retrospective study done by Wollega University in Neqemte General hospital among 315 TB patients registered from 2012-2016 show that 54(17.01%) are cured, 206(65.4%) completed treatment, 24(3.5%) had treatment failure, 11(3.5%) defaulted, 20(6.3%) were died. The overall treatment success rate of the TB patients was 82.5%. (27).
The study conducted in Debre Tabour general hospital done from 2008-2016 show that the overall successful treatment outcome was 90.1% (672) (cured and treatment complete) and 9.9%(74) (death and failure) were unsuccessful treatment out come from total of 985 patients included in nine year retrospective study. (28).
Five year retrospective study result in 2019 on TB patient registered from 2011-2015 in Harar the overall treatment success was 92.5%. (29).
In 2018 ten year retrospective study in Asella referral hospital was done on patient taking treatment and registered from 2004-2014 .According to this study result the overall treatment success rate was 81.7% (1434) from a total of 1755 patients included in the study (30).
2.2 .Determinant factors
Factors related to socio demographic characteristics of the patients
I China, Turk, Pakistan and Uzbekistan treatment outcome of TB patient negatively associated with the age of patients above 35 years old (21, 22, 31, 32). Another study result in Limpopo and Ethiopia show older ages above 65 years and youngers below 14 years were less likely treated (15, 29).
Different study result shows males were less likely treated than females (25, 26, 29, 33).
Weight of the patient is significantly associated with treatment outcomes. Those weight categories 50-70.9 kilograms were less likely treated un successfully compared to patient with weight categories of 40-54.9 kilograms (34).
Weight gain and weight loss between diagnosis and second phase of treatment associated with good and poor treatment out comes respectively (35-38)
Factors related to HIV Co infection
In Nigeria the study done in 2016 identifies the treatment success rate in TB HIV co infected patients was 9.5% lower than HIV negative TB patients (39). In addition to this finding similar study done in Limpopo shows adverse treatment outcome were high in TB HIV patients than the corresponding HIV negative patient (15).
In South Africa unsuccessful treatment outcome was recorded 24.5% for co infected patients and 15.3% for HIV negative patients. HIV positive TB patients are 2.35 and 1.8 times at risk for unsuccessful TB treatment out comes in 2009 and 2012 respectively (40).
Treatment success rate of TB HIV patient was 88.2% while, 93.6% in HIV negative patients in Ethiopia. On the other way, the cure rate is lower 10.1% and 24.2% in TB HIV patients and HIV negative TB patients. The death rate was also higher in co morbidity and no co morbidity patients 8.3% and 2.5% respectively (41).
Another study’s conducted in 2012, 2016, 2018 at different part of our country shows poor treatment outcome was significantly associated with HIV comorbidity (29, 42, 43).-
Factors related to treatment of the patient
The study done in Turk and Uzbekistan shows the treatment success rate was significantly associated with previous history of patient treatment. Previously treated patient by TB drugs were less likely to be treated successfully (21, 31).
Meta-Analysis done from 2005-2017 in Ethiopia and another study’s in northern Tigray,Gambela and Gondar shows previous history of TB patient would affect the current treatment out comes negatively (13, 42, 44, 45)
Factors related to type of TB
Among pulmonary TB patients in china in 2018 the treatment success rate of pulmonary positive was lower (92.02%) compared with pulmonary negatives (95%) (19).
Extra pulmonary had 3.175 times higher probability of un successfully treated than from all form of TB patients in Gondar University (34).
Patient with positive smear result at the end of second month of treatment had higher risk of unsuccessfully treated (36, 46, 47)
2.1.2 Conceptual framework
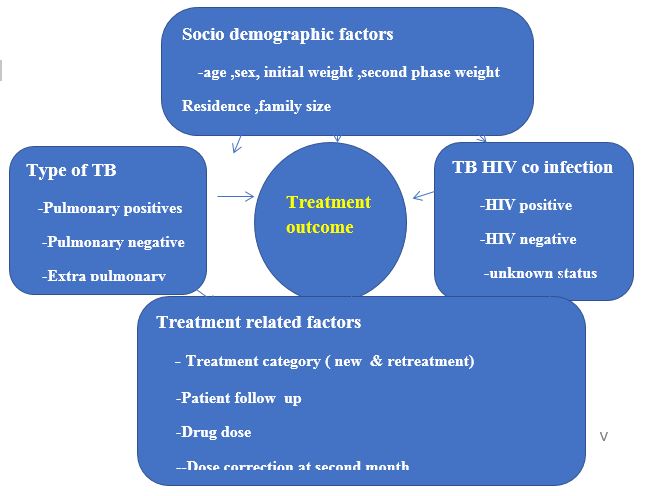
Figure 1: Conceptual framework for determinants of treatment out comes among TB patients developed by reviewing different literatures
3. Objective
To identify Determinants of treatment outcome among Tuberculosis patient in Jeju woreda, Arsi zone oromia regional state Ethiopia 2019
4. Methods and Materials
4.1. Study design and period.
Institution based retrospective case control study was conducted from September 4-14/2019 on TB patients who took treatment in government health facilities from June 28/ 2009 to June 27/2018 .
4.2. Study area
The study was conducted in Jeju woreda, Arsi Zone Oromia regional state, which is 82KM away from Assela town, capital city of Arsi Zone and 182KM from Addis Ababa. According to the 2018 vital statistics report, the woreda had 151506 total population and 31563 households. There are 26 rural Keble’s and 3 Urban Administrative Keble in the woreda. Dega is the major weather condition (47%). Weina dega and kola shares 33% and 20% respectively. There are 4 health centers and 26 health posts in the woreda. All health centers are diagnostic and provide DOT.
4.3. Source and Study population
4.3.1. Source population
All TB patients on anti TB treatment in Jeju woreda health facilities.
4.3.2. Study population
Selected TB patients registered in government health centers from June 28/ 2009 to June 27/2019 on anti TB treatment in government health facilities in Arsi Jeju Woreda would be included in the study.
Inclusion criteria:-
All TB patients registered on TB registration book and taking their treatment at government health facilities in the study area.
For patient taking treatment more than one the recent time of treatment was included in the study.
Exclusion criteria:-
Patient transferred out of the woreda to follow the treatment, unknown treatment outcome and drug resistance TB.
4.4. Sample size and sampling procedures
4.4.1. Sample size determination
The sample size was determined by using Epi info version7 Fleiss continuity correction formula
The following Assumptions used
Power=80%
Confidence interval=95%
Ratio of control to case=4:1
n=sample size in each group in case and controls
p1=proportion of expose in case
p2=proportion of expose in control
By taking the study result conducted in Dire Dawa Administration and Harari regional State, Eastern Ethiopian Intuitional based case control study design using the patients' record in 6 TB clinics providing DOT. The sample size was calculated depending on factors of exposure in case and control (46)
Exposure to lack of contact persone in case and control
p1= 42.73% and p2= 28.5% .n =116 and 464 case and control respectively . Total=580
Exposure to pulmonary negative TB type in case and control
p1= 47.3% and p2= 32% .n=106 and 422 case and contro respectively. Total=528
Exposure to smear posotive at second month in case and control
p1= 35.4% and p2= 4% .n=16 and 72 case control respectively.Total=78
therefore the largest sample was taken to increase the representativenes of the study which is 580. By ading 10% non response rate on each case and control total sample size requred for this study was 636 .
|
Determinants /exposure factors |
percentage of exposed in the previous study |
calculated sample size requred for curent study |
|||
|
control |
case |
control |
case |
total |
|
|
Exposure to lack of contact person |
28.5% |
72.73% |
464 |
116 |
580 |
|
Exposure to pulmonary negative TB |
32% |
47.3% |
422 |
106 |
528 |
|
Exposure to smear posotive at second month |
4% |
35.9% |
62 |
16 |
78 |
Table 1: sample size calculation
4.4.2. Sampling procedure
The desired sample size would selected from all health centers (Arboyye, Adis Hiwot, Bollo,and Denneb guddo) in Arsi zone Jeju woreda health centers providing DOT. The total patients registered and taking their treatment from June 28/ 2009 to June 27 /2018 in Jeju woreda were 2683 (Arboyye Health center 1073,Bollo Health center 654, Adis Hiwot Health center 517 and Denneb Guddo Health center 436) . Patient would selected by stratified random sampling technique based on the total sample size (636). For each health center proportion allocation formula was used.
Therefore the sample size required from each health center was calculated by proportion allocation formula:-
Sample size =niN*n
where ni =Total patient registered in the health center
N=Total patient registered in the woreda
n=Total sample size
Sampling procedures by graph
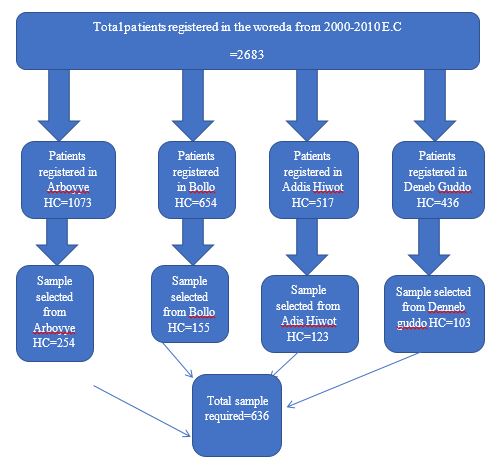
Figure 2: Schematic Sampling procedure for TB patients selected from each health centers for the study
4.5 Variables of the study
4.5.1. Dependent variable:
treatment outcome
4.5.2. Independent variables
Socio demographic factors
Sex
Age
weight
residence
Patient factors
Type of TB
Pulmonary positive
Pulmonary negative
Extra pulmonary
treatment category
New
Retreatment
HIV/AIDS co infection
Positive
Negative
Not known
4.6. Operational definitions and terms
The treatment outcome of patients was categorized according to the national TB and leprosy control program guidelines: cured, treatment completed, treatment failed, and defaulter, lost to follow up and died (48) .
In this study good /successful treatment outcomes (cured +completed) and poor treatment out comes (died, failure and defaulter) were considered as control and case respectively.
Successful treatment outcome: - if TB patient were cured or completed treatment with resolution of symptoms.
Unsuccessful treatment outcome: - if treatment of TB patients resulted in treatment failure, default or death.
4.7. Data collection procedures
The data was collected from DOT registration book developed by Federal ministry of health by using prepared checklists. The data collectors were 4 Clinical nurses who were trend on how to proceed for data collection.
4.8. Data quality assurance
The checklist was prepared originally in English. Training was provided for data collectors and Pre-test was done in Sire woreda before data collection on 5% of the sample selected randomly to check the appropriateness and completeness of the checklist to ensure data quality.
4.8. Data processing and analysis
Data was entered using EPI INFO version-7 statistical software and then imported to SPSS Version 21 for analysis. Descriptive statistics was used in the study using statistical measurements, Frequency tables, graph and proportion. Bivariate and multivariate logistic regression analyses were used with 95% confidence interval. Variables with p value <0.2 in bivariate analyses were moved to multivariate analyses. Odd ratio was used to see the strength of association between dependent and independent variables. Variables with P-value <0.05 in multivariate analyses was considered as statically significant.
4.9 Ethical considerations/Statement
The study was conducted after getting permission/ clearance from the ethical review board of Arsi University. Permission was signed from Jeju woreda health office to conduct the study.
4.10. Dissemination of results
The final result is presented for partial fulfillment of the degree of Master of public health to Arsi University collage of public health. Finding of the study was submitted to Arsi University department of Public Health, Jeju Woreda health office, Jeju woreda health centers and Arsi Zone Health department.
5. Result
Socio-demographic characteristics of study subjects
This study enrolled 509 controls with successful treatment out comes and 93 cases with poor treatment out comes. From total of 602 case and controls included in the study the response rate was 95% (100% for controls and 73% for case).majority of patient, 276(45.8%) of controls and 53(8.8%) of cases were males. The majority age of the subjects in controls were between 15-24 years 140(23.3%) and 35-44 years for cases groups. Higher proportion of the patient 446(74%) of controls and 85(14.1%) of cases were from rural residence.
|
Patient characteristics |
Controls (successfully treated) n (%)
|
Case (unsuccessfully treated) n (%) |
Total n (%)
|
|
|
Number of patients |
509(100) |
93(73) |
602(95) |
|
|
sex of the patient |
male female |
276(45.8) 233938.7) |
53(8.8) 40(6.6) |
329(54.7) 273(45.3) |
|
Age of the patient in years |
≤ 5-14 15-24 25-34 35-44 45-54 55-64 >65 |
10(1.7) 54(9) 140(23.3) 127(21.1) 81(13.5) 55(9.1) 30(5) 12(2) |
1(0.2) 5(0.8) 17(2.8) 17(2.8) 26(4.3) 10(1.7) 9(1.5) 8(1.3) |
11(1.8) 59(9.8) 157(26.1) 144(23.9) 107(17.8) 65(10.8) 39(6.5) 2093.3) |
|
Residence
|
Urban Rural |
63(10.5) 446(74) |
8(1.3) 85(14.1) |
71(11.8) 531(88.2) |
|
Weight of the patient in KG |
<10 11-19 20-29 30-39 40-54 >55 |
6(1) 20(3.3) 26(4.3) 93(15.4) 271(45) 93(15.4) |
1(0.2) 3(0.5) 7(1.2) 18(3) 46(7.6) 18(3) |
7(1.2) 23(3.8) 33(5.5) 111(18.4) 317(52.7) 111(18.4) |
|
Family size of the patient |
1-2 3-5 >5 not known |
33(5.5) 35(5.8) 29(4.9) 412(68.40 |
12(2) 17(2.8) 31(5.1) 33(5.5) |
45(7.5) 52(8.6) 60(10) 445(73.9)
|
Table 2: Distribution of Socio demographic characteristics of patient in Arsi Jeju Woreda from June 28/2009 to June 27/2018 ,2019 CI 95% ,N=602 (509 controls and 93 case)
Clinical characteristics of the study subjects
During diagnosis, majority of study subjects in the control group 29.2% and 6.8% of cases had pulmonary negative and pulmonary positive TB respectively. Higher proportion 80.4% of controls and 13.3 % of cases were newly enrolled TB patients. HIV positive TB patients were 1% in controls and 1.8% in cases.
|
Patient characteristics |
Control group [n (%)]
|
Case group [ n (%)]
|
|
|
Tuberculosis type
|
Pulmonary Positive Pulmonary negative Extra pulmonary |
17
4(28.9) 176(29.2) 159(26.4) |
41(6.8) 17(2.8) 35(5.8) |
|
Treatment category |
New case Re treatment /previously treated case |
484(80.4) 25(4.2) |
80(13.3) 13(2.2) |
|
HIV status |
Positive Negative Not known |
6(1) 491(81.6) 12(2) |
11(1.8) 76(12.6) 6(1) |
Table 3: Distribution of TB patient and their clinical characteristics in Arsi Jeju Woreda from June 28/2009 to June 27/2018 ,2019 , CI 95% ,N=602 (509 controls and 93 case)
Determinant factors of TB treatment out comes
This study point out that there was statistically significance association between TB treatment out comes and predictor variables.
In bivariate analyses ,age >65 years old ,weight loss at second months of treatment,>5families ,HIV co-infection, patient have no follow up, patient with no dose correction at second month, retreatment category, pulmonary positive TB, self-referred patients and second month smear positive result were determinant factors .
In multivariate analyses, patients those have no dose correction during second phase treatment (AOR=17.949 CI 95% 5.528-91.326), decrease weight during second phase of treatment (AOR =10.68 CI 95% 3.076-37.098 ), HIV co-infection and positive smear result at the end of second month were factors significantly associated with poor treatment out comes.
Weight gain at second phase of treatment, corrected second phase drug dose, HIV negative and negative smear result at the end of second month were determinant factors for good treatment out comes.
|
Associated factors |
Controls [n (%)] |
Case [n (%)] |
COR |
P value
|
|
|
Age of the patient in years |
≤ |
10(1.7) |
1(0.2) |
|
.003 |
|
5-14 |
54(9) |
5(0.8) |
0.926(.098--8.790) |
.947 |
|
|
15-24 |
140(23.3) |
17(2.8) |
1.214(.146--10.080) |
.857 |
|
|
25-34 |
127(21.1) |
17(2.8) |
1.339(.161--11.119) |
.787 |
|
|
35-44 |
81(13.5) |
26(4.3) |
3.210(.392--26.280) |
.277 |
|
|
45-54 |
55(9.1) |
10(1.7) |
1.818(.209--15.817) |
.588 |
|
|
55-64 |
30(5) |
9(1.5) |
3.00(.337--26.710) |
.325 |
|
|
>65 |
12(2) |
8(1.3) |
6.667(.708--62.73)8 |
0.097 |
|
|
Family size of the patient |
1-2 |
33(5.5) |
12(2) |
|
.000 |
|
3-5 |
35(5.8) |
17(2.8) |
1.336( .555---3.216) |
.519 |
|
|
>5 |
29(4.9) |
31(5.1) |
2.94(1.279---6.758) |
.011 |
|
|
not known |
412(68.40 |
33(5.5) |
.220(.104--.466 ) |
.000 |
|
|
Continuation phase weight compared with initial weight |
Increase |
371(63.5) |
41(7) |
|
.000 |
|
Decrease |
35(6) |
17(2.9) |
4.395(2.264--8.531) |
.000 |
|
|
Stable |
44(7.5) |
5(0.9) |
1.028(.386--2.739 ) |
.956 |
|
|
not evaluated |
59(10.1) |
12(2.1) |
1.840(.914--3.704 ) |
.087 |
|
|
HIV status |
Positive |
6(1) |
11(1.8) |
|
.000 |
|
Negative |
491(81.6) |
76(12.6) |
.084(.030--.235)
|
.000 |
|
|
|
Not known |
12(2) |
6(1) |
.273(.067--1.102) |
.068 |
|
Patient follow up |
followed |
407(67.6) |
61(10.1) |
|
|
|
not followed |
102(16.9) |
32(5.3) |
2.093(1.296--3.382) |
.003 |
|
|
Dose correction during continuation phase |
done |
494(85) |
66(11.4) |
|
|
|
not done |
14(2.4) |
7(1.2) |
3.742(1.458-9.609) |
0.006 |
|
|
Treatment category |
New case |
484(80.4) |
80(13.3) |
|
|
|
Re treatment case |
25(4.2) |
13(2.2) |
3.146(1.546-6.403) |
0.002 |
|
|
Tuberculosis type
|
Pulmonary Positive |
174(28.9) |
41(6.8) |
|
0.010 |
|
Pulmonary negative |
176(29.2) |
17(2.8) |
0.410(0.224-0.749) |
0.004 |
|
|
Extra pulmonary
|
159(26.4) |
35(5.8) |
0.934(0.567-1.540) |
0.789 |
|
|
Source of initial referral |
HEW |
71(11.8) |
19(3.2) |
|
0.000 |
|
Self |
178(29.6) |
49(8.1) |
1.029(0.566-1.869) |
0.926 |
|
|
HW |
102(16.9) |
14(2.3) |
0.513(0.241-1.090) |
0.083 |
|
|
Second month sputum result |
positive |
0(0) |
6(2.8) |
|
0.000 |
|
negative |
163(77.3) |
19(9) |
0.000 |
0.999 |
|
|
not known |
11(5.2) |
12(5.7) |
0.00 |
0.999 |
|
Table 4: Bivariate analyses of Factors associated with unsuccessful treatment out comes among TB patient from June 28/2009 to June 27/2018 in Arsi Zone Jeju woreda health centers , 2019 CI 95% n=602 (509 controls & 93 case)
|
Associated factors |
Control [n (%)] |
Case [n (%)] |
AOR |
p value |
|
|
Continuation phase weight compared with initial weight |
Increase |
371(63.5) |
41(7) |
|
0.001 |
|
Decrease |
35(6) |
17(2.9) |
10.681(3.076---37.098) |
0.000 |
|
|
Stable |
44(7.5) |
5(0.9) |
2.288(0.491---10.656) |
0.292 |
|
|
not evaluated |
59(10.1) |
12(2.1) |
7.4165(1.631—33.718) |
0.10 |
|
|
Dose correction during continuation phase |
done |
494(85) |
66(11.4) |
|
|
|
not done |
14(2.4) |
7(1.2) |
17.949(3.528-91.326) |
0.001 |
|
|
HIV status |
Positive |
6(1) |
11(1.8) |
|
0.075 |
|
Negative |
491(81.6) |
76(12.6) |
0.050(0.003-0.759) |
0.031 |
|
|
Not known |
12(2) |
6(1) |
0.124(0.004-4.103) |
0.242 |
|
|
Second month sputum result |
positive |
0(0) |
6(2.8) |
|
0.020 |
|
negative |
163(77.3) |
19(9) |
0.000 |
0.999 |
|
|
not known |
11(5.2) |
12(5.7) |
0.000 |
0.999 |
|
Table 5: multivariate analyses of Factors associated with unsuccessful treatment out comes among TB patient from June 28/2009 to June 27/2018 in Arsi Zone Jeju woreda health centers , 2019 CI 95% n=602 (509 controls & 93 case)
6. Discussion
A case control study with 93 case and 509 controls was conducted to identify determinants of treatment out comes in four health centers providing DOT in Arsi zone Jeju woreda. This study shows in multivariate analyses patients with decrease weight at second phase of treatment compared with initial weight, patient with uncorrected second phase dose, HIV positive TB patients and smear positive at the end of second month of treatment were determinant factors for unsuccessful treatment out comes.
This study result shows the patient with decreased weight between initial treatment and second phase of treatment had greater chance to be unsuccessfully treated (AOR =16.539 CI 95% 3.008-90.923 ), on the other ways patient with weight gain between initial treatment and second phase of treatment shows better chance for successful treatment out comes. This result was consistence with finding of previous studies conducted in other settings (35-38).
The result of this study shows success of TB treatment outcome are significantly different between HIV positive and HIV negative TB patients. In this HIV infection was one of the risk factor for unsuccessful TB treatment out comes. The finding of this study was in line with previous studies conducted in Nigeria, South Africa and Ethiopia (39-41).
The result this study shows that sputum conversion at the end of second month of treatment for pulmonary positive TB patients was significantly associated with success of TB treatment out comes. Patient with positive smear result at the end of second month of treatment have higher risk of unsuccessfully treated. Similar result was obtained from studies conducted in different part of Ethiopia (36, 46, 47)
7. Limitation of the study
Since data was collected from secondary source it can’t assessed different factors that can affect TB treatment outcomes positively or negatively, including life style, presence or absence of chronic disease (hypertension, Diabetics, heart disease, liver disease etc.), educational level, nutritional status, etc.
It does not include those patients taking their treatment out of the study area (transferred out patient).
8. Conclusion
Decreased Weight during second phase of treatment compared with initial weight, uncorrected drug dose at second phase of treatment, HIV comorbidity and positive smear result at the end of second month were factors independently associated with poor treatment out comes of TB patients.
9. Recommendation
To the health centers
Patient losing weight during treatment, positive sputum result at the end of second month, and HIV positive TB patients should be more closely followed as they were at risk of unsuccessfully treated.
Patient weight must be measured regularly and taking corrective action if important if the patient weight goes back.
The required data needed should be registered on TB registration book.
Dose correction was important done during continuation phase of treatment and appropriate dose should be given to the patient based on weight.
To the zonal and woreda health office Regular supervision and monitoring of the DOT strategy at health facilities is mandatory.
To the researchers Other study should be done in combination of data from primary and secondary source to get more accurate results.
ACRONYMS/ ABRIVAITION
AIDS---Acquired Immune Deficiency Syndrome
AFB---Acid Fast Basils
ART---Anti Retro Viral Treatment
ATT---Anti Tuberculosis Treatment
DOT---Direct Observed Therapy
HC---Health Center
HEW---Health Extension Workers
HIV----Human Immune Vires
HW---Health Workers
LTF---Lost To Follow up
MBT---Micro Bacterium Tuberculosis
TB---Tuberculosis
TO---Treatment Outcome
TTS---Tuberculosis Treatment Supporters
WHO---World Health Organization
Acknowledgement
I would like to acknowledge Arsi University Collage of public health giving this chance to me to do this thesis. I want to acknowledge Mr. Teresa Kisi and Mrs. Yealemwork Kerie my advisers for helping me since the start of developing the proposal until the end of this research.
I wish to express my special thanks to Jeju woreda health office and workers for their support and encouragement.
My special thanks also go to my families, friends and classmates for their support while doing this study.
Last but not list I would like to thank the data collectors and supervisors