Jenny Molano Caro1*, Crystian Borrero-Cortes2, Jorge Lizarazo Rodríguez3
1Specialist in Internal Medicine, Gastroenterology and Digestive Endoscopy Pontificia Universidad Javeriana. Emdiagnostica Medical Director. Carrera 18, 84-11 Consultorio 402. ORCID 0000-0001-9013 3189
2Specialist in Anesthesiology and Resuscitation. Universidad Nacional de Colombia. Occasional Professor Universidad Nacional de Colombia. Emdiagnostica Anesthesiologist. ORCID 0000-0002-9285-9984.
3Specialist in Internal Medicine, Gastroenterology and Digestive Endoscopy. Universidad Nacional de Colombia, Emdiagnóstica Gastroenterologist. ORCID 0000-0001-6250-2821
*Corresponding author: Jenny Molano Caro, Specialist in Internal Medicine, Gastroenterology and Digestive Endoscopy Pontificia Universidad Javeriana. Emdiagnostica Medical Director. Carrera 18, 84-11 Consultorio 402. ORCID 0000-0001-9013-3189.
Received: January 18, 2021
Accepted: January 27, 2021
Published: February 05, 2021
Citation: Jenny M Caro, Crystian B Cortes, Jorge L Rodríguez. “Application of Practice Ambulatory Digestive Endoscopy Protocols During the Covid- 19 Pandemic. how we are doing in Real Life”. J Gastroenterology and Hepatology Research, 2(1); DOI: http;//doi.org/03.2021/1.1004.
Copyright: © 2021 Jenny Molano Caro. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
In Colombia, since March 2020, when the first case of SARS COV-2 was identified, normal functioning of health systems was affected, including gastroenterology and digestive endoscopy units. As majority of countries, mandatory confinement with suspension of outpatient diagnostic procedures was implemented, initially during seven weeks. Outpatient gastroenterology units remained closed and had to adapt physically and logistically to be able to perform endoscopic procedures to patients with relevant symptoms for whom endoscopic procedures could have an impact on the prognosis and outcomes in medium and short term intime-sensitive diseases. Experience shared by countries previously affected from December 2019 to April 2020 and the development of guidelines and recommendations by different scientific societies were invaluable resources for countries just starting with the pandemic. Remote consulting, application of scales to filter, prioritize and ponder cases based on clinical criteria through adequate planning has been the basis of our endoscopy unit for responding to the challenges generated within a complex and unpredictable scenario such as current one.
Introduction
The pandemic declared by the World Health Organization [1] (WHO) on March 11, 2020 by the new coronavirus (SARS-Cov-2) and that causes the Coronavirus Disease 2019 (COVID-19) required the adaptation of health systems worldwide to avoid its collapse. The functioning of gastroenterology and endoscopy units was particularly affected by the possible infection transmission attributed to the aerosols during endoscopic procedures, the detection of viral particles in feces and initially by the suspicion of transmission through endoscopy equipment, which was finally discarded recognizing that the rigorous cleaning and disinfection of the equipment is sufficient to avoid this risk.
In Colombia, the national government decreed mandatory quarantine with successive extensions from March 2020 in seeking to delay the rapid rise of cases. During a first absolute quarantine (7 weeks), only urgent procedures could be performed at the hospital level, causing the holding back of patients requiring outpatient endoscopic procedures. In May, reopening was allowed, without specifying for how long. This situation made it essential for the provision of outpatient services to determine how, when and which patients would be treated, in what order, how exposure to risk would be controlled so as not to outweigh the benefit, and how available resources would be used optimally. Delaying diagnosis in time-sensitive pathology in a country as Colombia, where colon and gastric cancer are among the top five in prevalence, incidence and mortality [2], along with the impact on clinical outcomes that an early and timely diagnosis could have, were sufficient reasons for our unit - EMDIAGNOSTICA - developed a comprehensive action plan that would allow the performance of outpatient endoscopic procedures. Early in March, remote consulting modality was established, together with the application of scales to filter, prioritize and ponder cases based on clinical criteria with a careful planning of the expenditure was the basis to respond to the challenges generated. On this scenario EMDIAGNOSTICA in Bogota-Colombia, developed an action plan, published in the Colombian Journal of Gastroenterology (Rev Col Gastroenterol. Bogotá.2020; 35(3):287-297) [3] with protocols, processes, and procedures that made it possible to respond to the contingency in a planned and orderly manner applicable to all phases of the pandemic. A multidisciplinary group of professionals (gastroenterologists, anesthesiologists, lawyers, nurses, and financial advisors) participated in the plan, which finally wrote a series of recommendations to return to the provision of services based on a scheme of logistical and physical infrastructure adaptations, objective prioritization of procedures, adjustments to the availability of supplies (including availability of personal protective equipment (PPE)), and a possible shortage of analgesics and sedatives; always maintaining the internationally recommended quality standards for upper endoscopy, colonoscopy and sedation.[4,5,6]
Experience shared by affected countries from December 2019 to April 2020 along with national and international guidelines and recommendations [7,8,9,10,11,12,13,14,15,16,17] were invaluable resources for countries as we began to experience the pandemic. Scientific societies worldwide made great and generous efforts to unify criteria, focusing especially on diagnostic procedures at intrahospital environment, establishing guidelines and protocols to define those who should perform such procedures, giving priority to those classified as urgent.However pandemic lasted beyond any established planning while the emergency services were overwhelmed, patients refused to attend the emergency department and waiting time to reach the "new normal" was prolonged.
Repici and cols [16] at the beginning of 2020 published recommendations for hospital safe operation of endoscopy units, with emphasis on personal protection elements, individual COVID-19 risk of patients and prevention of spread of infection. In March 2020, the Canadian Gastroenterological Association drafted guidelines [7].to reduce and delay the transmission of COVID-19. These guidelines classified all high endoscopic procedures as high risk for the spread of the virus regardless of the patient's individual risk, insisting on the need to classify the procedure to be performed as essential or not.
In March, AASLD, ACG, AGA, and ASGE published the Joint GI Society Message [8] setting for recommendations to scheduling non-urgent elective procedures, taking into account priority, such as screening for suspected cancer, need for prosthesis removal, and assessment of relevant symptoms. Thompson [9] described strategies for an orderly step-by-step approach and classified non-urgent procedures into those to perform and those to postpone, highlighting the relevance of telemedicine to the success of these strategies.APSDE [13] published perhaps one of the most important position statements establishing strategies for pre-selection and filtering of patients, classifying endoscopic procedures as urgent, semi- urgent and elective and determining their scheduling according to the behavior of local epidemiological curves of COVID-19. This document was the basis for the establishment of contingency measures in EMDIAGNOSTICA.
Shortly thereafter, ASGE [14,15] published guidelines for reopening endoscopy units after the COVID-19 pandemic aiming to decrease the risk of infection during a gradual reopening. It established strategies for estimating the risk of infection in patients, room preparation, appropriate use of PPE, reprocessing of equipment, post-procedure follow-up, and classified procedures in urgent, semi-urgent, and elective, considering co- morbidities and establishing activities in every step of the process.
In May, the World Endoscopy Organization [18] called attention to the potential danger of delaying diagnosis in some patients and the importance of recognizing the benefit over the risk in performing endoscopic procedures. Additionally, it highlighted the importance of strict follow-up for patients with deferred procedures, differentiating an elective procedure from one that is not indicated.
The AGA[19] issued recommendations for gastrointestinal procedures during the pandemic in August, emphasizing the need to define whether a procedure is time-sensitive and therefore whether its cancellation could significantly affect the prognosis or progression of the disease; it also established an 8-week maximum period in which such procedures should be performed.
The action plan in force in EMDIAGNÓSTICA since April 2020, considered first a risk estimation for the assistance and administrative personnel of the unit, which allowed to divide the work group in two, one for face-to-face activity in the physical plant and another for assistance in teleworking. Additionally, in order to limit the exposure of the members of the on-site group, this group was divided into two subgroups for the rotating provision of services. Multiple virtual meetings were held for education on posture and withdrawal of PPE and the continuous availability of these elements was guaranteed.
Educational videos and guides for patients are available on our website www.emdiagnostica.com. All the documents generated or adapted for the contingency are summarized in TABLE 1. Due to the high percentage of asymptomatic patients, it was agreed to consider all of them as suspects of active infection and therefore protective measures are routinely applied in all cases.
In order to modulate the risk of infection the physical plant was adjusted according to the recommendations of Cennamo et al [17]. ensuring adequate ventilation, availability of negative pressure, HEPA filters and sufficient air changes (15 per hour). Common areas and work cubicles were demarcated with warning lines according to the degree of exposure to drops and aerosols and safe areas were established for posture and removal of PPE.
Since March, the gastroenterology clinic is carried out by telemedicine modality, determining which patients require face- to-face attention and establishing the relevance of performing diagnostic endoscopic procedures and prioritizing them according to the criteria defined in TABLE 2 and FIGURES 1 and 2. Procedures scheduling is based on the gastroenterologist's criteria according to the diagnostic probability of cancer, the presence of alarm symptoms and the risk/benefit balance during the pandemic. In addition, the possibility of reducing hospital overload by relaxing the criteria for performing endoscopic procedures at the outpatient level for specific situations such as elderly patients with controlled comorbidity, hemodynamic stability, and the presence of melena in the context of overuse hospitals has been taken into consideration.
During rising phase in the epidemiological curve, three priority “ P” groups were established; Priority-1, those that in the opinion of the gastroenterologist needed to be done in the two weeks following the consultation, Priority-2, to be done between weeks 3 and 4, and Priority-3, to be done between weeks 5 and 8, according to the criteria listed in FIGURE 1. It was established that during curve fall, "D”, necessary diagnostic procedures would be performed in symptomatic patients with risk factors, previously postponed high-risk screening and cancer follow-up for whom the risk of delaying the procedure was unacceptable. Also included were patients in whom the procedure was indispensable for taking on actions by other specialties. In the normalization stage, "N”, the diagnostic procedures considered necessary in patients without risk factors, the follow-up of low- risk lesions or those that allow wide follow-up margins in time, and the procedures for average risk screening were added. (TABLE 2, FIGURES 1 and 2). With regard to colonoscopies performed by fecal positive occult blood, the AGA recommendation was followed; however, after the recommended 6 months, it was considered that the colonoscopy should be performed from within group D after a discussion and individualization of the risk with the patient.
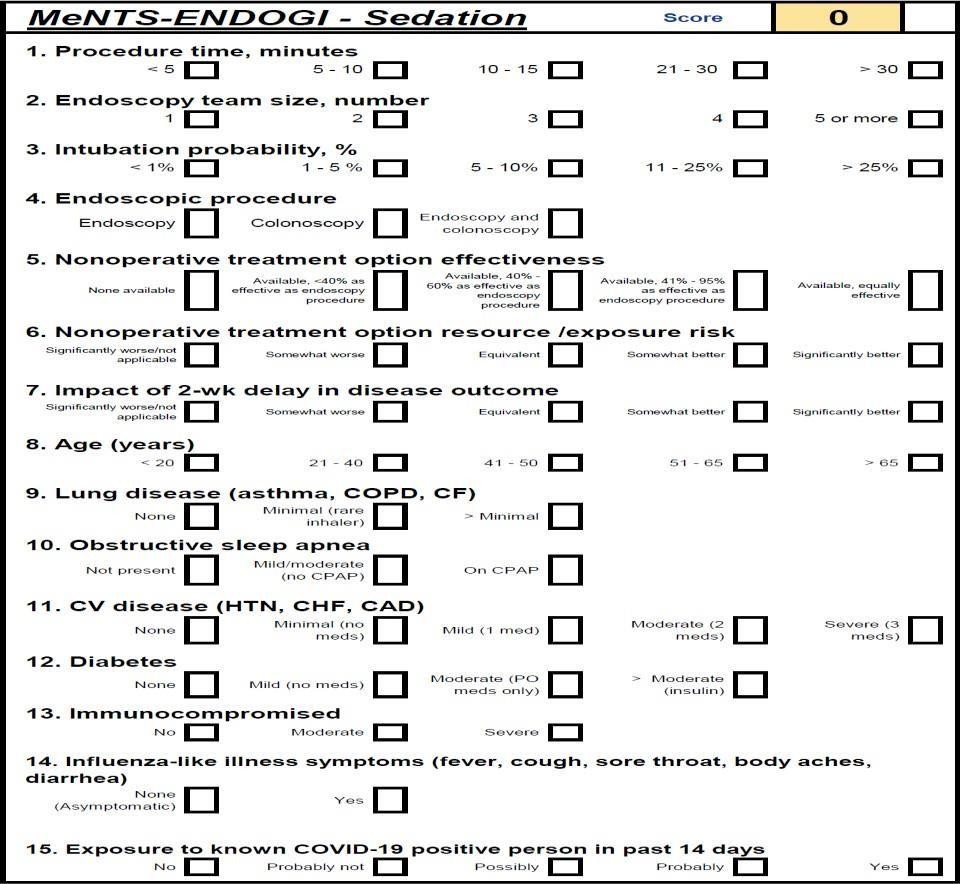
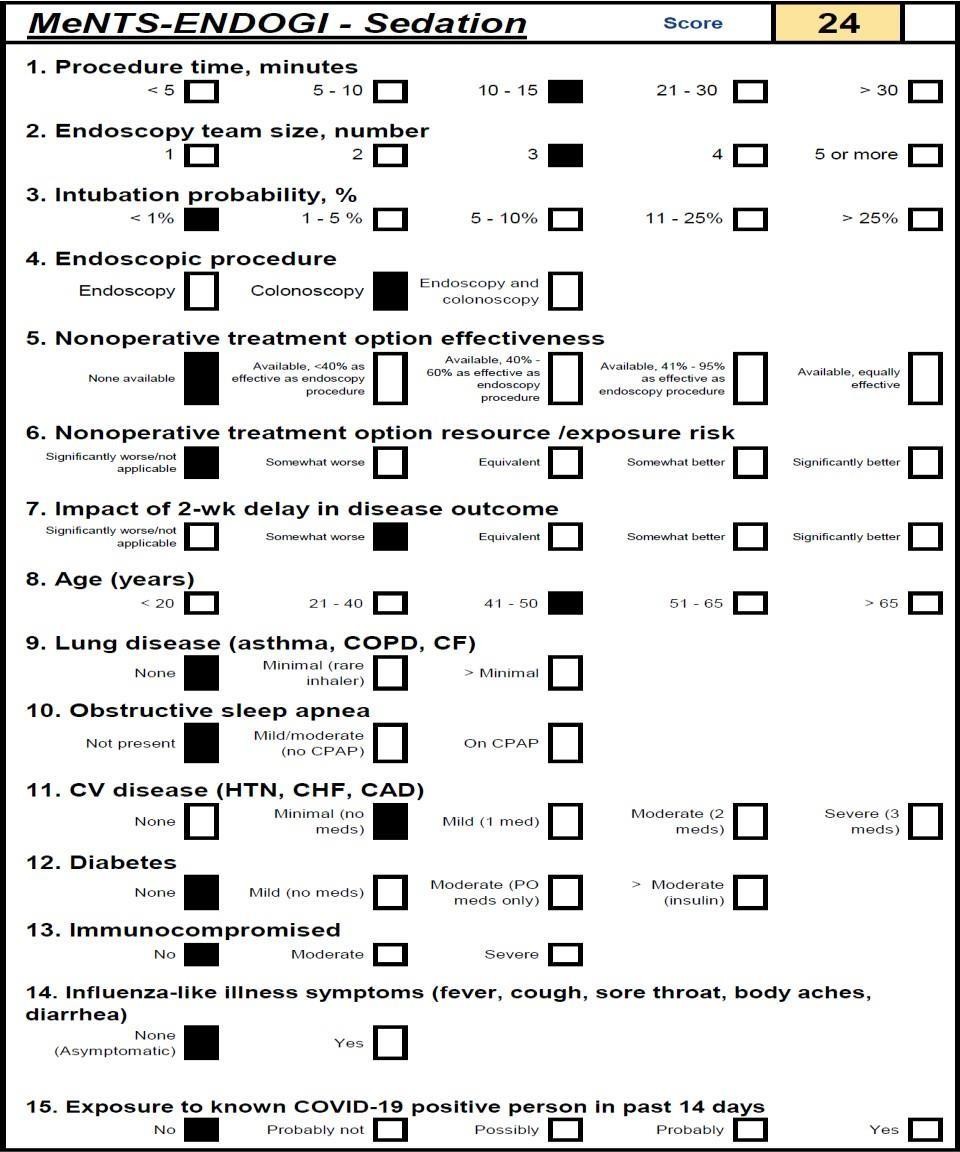
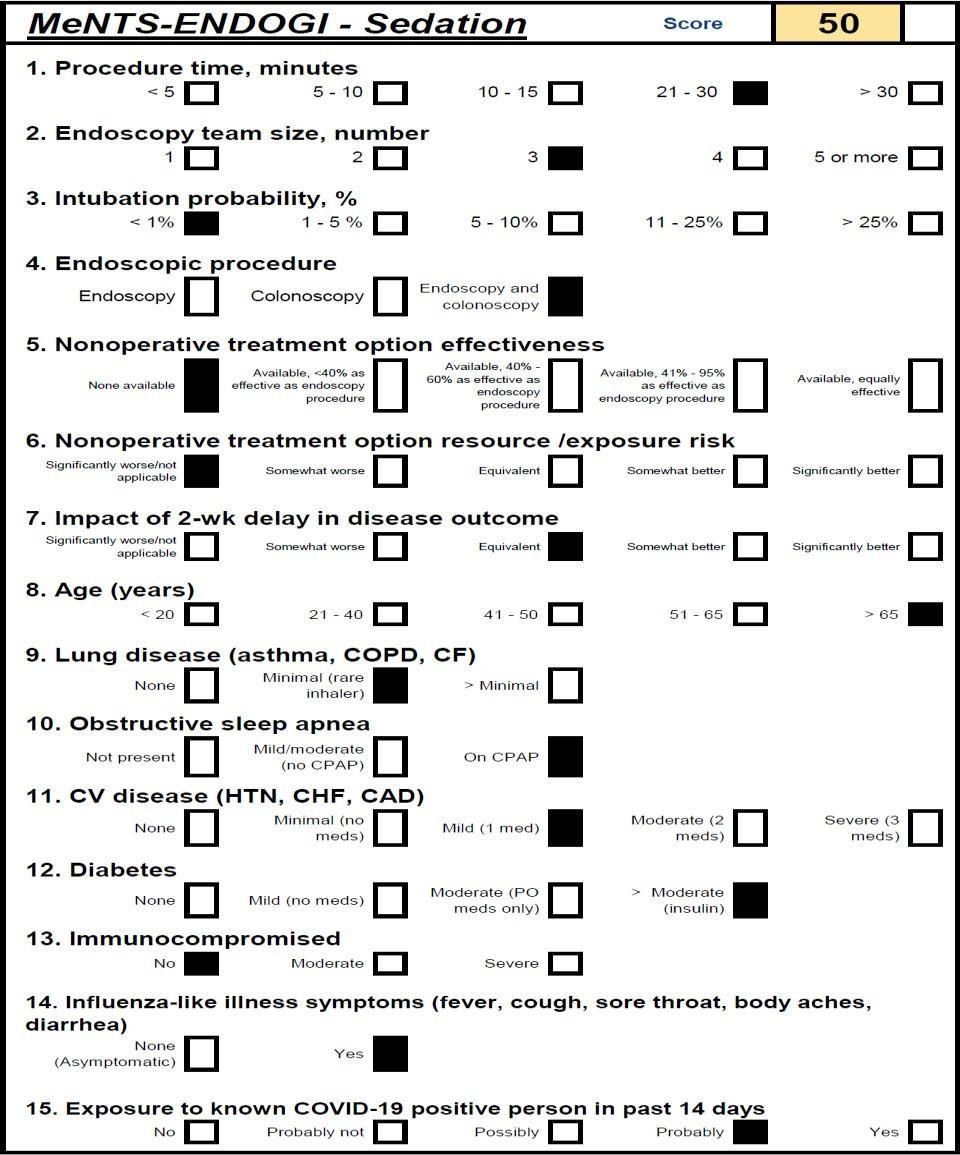
Between 24 and 48 hours prior to the procedure (depending on the case for endoscopy or colonoscopy) each patient is contacted by telephone to re-classify his or her risk and define the execution or postponement of the procedure. In case there is any doubt about the scheduling of the procedure or when it is postponed, the patient is scheduled for a remote consultation. By means of virtual care, in addition to defining the indication and timing of the procedure, the level of care during the pandemic is established using an adaptation of the MENTS scale published by Prachand et al.[20] to be applied in the scenario of ambulatory endoscopic procedures, named by us as MENTS-ENDOGI (FIGURE 3), establishing the safety of the ambulatory environment for a value of up to 45 points. For higher values, the recommendation was to refer the patient to an in-hospital level.
During the rising phase of the COVID-19 curve, we program alternately in each of the three available rooms using a maximum of 30% of the installed capacity, allowing ventilation, cleaning and disinfection of the area before each patient's admission. Progressively, during the curve's descent phase and when government guidelines allowed it, the use of the installed capacity was increased to 60% and now, since a new ascent phase was presented towards a new peak of the COVID-19 curve with an ICU occupation higher than 85%, the strategy for the curve's ascent was resumed.
The healthcare and administrative personnel involved in patient care always use a complete PPE endorsed and provided by the institution without allowing the use of external items, including elastomeric masks. The external anti-fluid gown is removed in a specific area of the unit and a new gown is always used with each patient.
In all procedures, the plastic barrier described by Dr. Luis Carlos Sabbagh [21] is used to isolate the patient from the care staff. The registration of quality indicators for the endoscopic procedure in the roadmap and verification of processes is always diligent and the resection of lesions (polyps) found is performed depending on their characteristics, the local occupation of ICU and individual risk.
Endoscopic procedures in the unit are performed under sedation administered by anesthesiologists. Before the pandemic it was usual to keep patients in a level II sedation according to the Practice Guidelines for Sedation and Analgesia by non- Anesthesiologist classification [22], but considering the need to decrease the risk of droplet and aerosol emission (cough reflex) during the crycopharyngeal pass, it was decided to administer the conventionally used drugs until a higher degree of sedation was achieved by adjusting the doses accordingly: Remifentanil (0.4 -5mcg/kg) and Propofol (1.5 - 2.5 mg/Kg). To mitigate the effect of apnea on desaturation and hypoxemia, the routine administration of oxygen by nasal cannula at 2 - 3 L/min oxygen for 3 minutes (below the isolation barrier) was protocolized. The patient is always motivated to breathe his vital capacity in each ventilatory cycle. In cases where the apnea could be accompanied by desaturation (SpO2 less than 90%) it was established as a plan of action to increase the oxygen flow to 5 L/min and perform airway permeability maneuvers. To date, only 0.04% of the cases have required oxygen administration by face mask with a four- handed airtight seal technique. No patient has required endotracheal intubation and 100% of the procedures have been successfully performed without compromising the safety of the care staff.
Since September 2020 and as a consequence of a substantial increase in the number of active cases of COVID-19 associated with a high occupation of ICUs, Colombia has experienced a relative lack of analgesic and sedative medicines. This forced the application of new pharmacological strategies for sedation. Currently, the unit uses a sedation scheme with Fentanyl (0.2 - 0.3 mcg/Kg) + Ketamine (0.1 - 0.2 mg/Kg) + Propofol (0.5 - 1 mg/Kg), which has maintained the quality of the sedation, the safety of the care staff and incidentally a shorter recovery time, less incidence of desaturation and less hemodynamic impact with changes in heart rate and blood pressure parameters not exceeding 3% of the baseline data of each patient have been found. These measures allow us to continue offering the sedation service using pharmacological resources in an optimal and responsible way.
All patients have been followed by telephone after the procedure to evaluate the appearance of symptoms or diagnosis of COVID- 19 at 7 to 14 days and complications after polypectomy between 12 - 48 hours. A survey on the degree of satisfaction and the perception of security during their stay in the unit is routinely applied to all telephone contacts with the patient.
Patients whose endoscopic procedures have been postponed have been monitored by remote assistance, establishing the best time for their performance by reclassifying them to P1, P2 or P3 due to the appearance of alarm symptoms or persistent symptoms despite treatment. Our staff meets on average every 2 weeks to evaluate and socialize results.
From May 11 to December 31, 2020, 3628 endoscopic procedures had been performed at EMDIAGNOSTICA. Eleven patients (0.30%) during follow-up reported symptoms that required ruling out COVID-19, confirming 5 positive cases (0.14%) that required only outpatient treatment; in 3 of these cases there was previous contact with positive cases for COVID-19 not reported by the patient, 1 worked as a pharmacy staff and the other had no known epidemiological risk factor. In none of the cases there was an associated outbreak among EMDIAGNOSTICA care or administrative personnel.
We are currently in the tenth month of the evolution of the COVID-19 pandemic in Colombia, in a new reality that deeply impacted the practice of ambulatory digestive endoscopy. The follow-up of the regulations and guidelines of the different scientific societies allowed us to restart and continue the assistance activity. Continuing with the provision of outpatient services, prioritizing non-urgent but time-sensitive procedures, is indispensable since early and timely diagnosis, clinical intervention on the diagnoses made, resolution of pathologies with therapeutic procedures by endoscopic or surgical means, and risk stratification have a significant impact on the prognosis of the disease and on the medium and long-term outcomes with benefits on the quality of life of patients, being able to access these services in a timely and safe manner, reducing anxiety and uncertainty. In addition, outpatient digestive endoscopy units contribute to decrease the demand for hospital care by maintaining timely coverage and access for patients who feel less exposed in the outpatient units. Follow-up surveys have shown a high degree of satisfaction and biosafety protocols have guaranteed the safety of care especially in the prevention of COVID-19 infection during digestive endoscopy procedures.
The prioritization scales and the application of the MENTS scale adapted to endoscopy (MENTS-ENDOGI) have been important to define which patients to schedule, when and where. Systematic records, patient follow-up, measures to reduce infection, diagnoses achieved, and new aspects related to medical legal liability are issues to be considered in future adjustments.
The shortage of medicines, especially those for sedation, resulting from their high demand in intensive care units worldwide was another challenge for the practice of digestive endoscopy requiring the adaptation of new sedation protocols. The results of the application of our new sedation protocol and the diagnostic data obtained according to the prioritization have been collected and will be socialized in future EMDIAGNOSTICA publications that will be presented as original paper.
The economic aspects (higher costs with fewer procedures) could come to threaten the stability of the institutions so objective strategies to filter, prioritize and balance the cases based on clinical criteria with a fair planning of expenditure have never been so important in a complex and unpredictable scenario asthe current one.
Pandemic Long duration , requirement of safety measures that can be exhausting, use of personal protection elements that require specific protocols for their adequate use, fear of getting sick, among other factors, increase possibility of development of burnout syndrome in health personnel, which has serious consequences as worker as patients. Dimitriuet [23] al found an average of 76% burnout in residents, particularly those under 35 years of age. Adequate organization of endoscopy units and good communication of the entire work team are necessary strategies to improve the perception of safety of health care workers and decrease the risk of burnout syndrome.
The COVID 19 pandemic has been a challenge to optimize the maximum available resources in all areas of health. Leadership, teamwork and the generosity of the global scientific community are fundamental elements in the search for solutions applicable to an unpredictable and variable scenario. It remains to be hoped that the initiation of vaccination will progressively return to normal care as the COVID 19 pandemic is brought under control.
|
|
Documents adapted, modified, or created for start-up in a pandemic era. |
|
|
|
COVID-19 Patient Training Booklet |
|
|
|
Informed consent for endoscopic procedures (Endoscopy, Colonoscopy, Polypectomy) |
|
|
|
Informed consent for face-to-face consultation. |
|
|
|
Informed consent for remote consulting |
|
|
|
Informed Consent to Sedation. |
|
|
|
Informed consent for escort. |
|
|
|
COVID-19 Health and Risk Statement for Patients, Escorts, Providers, Clients, Administrative and Care Staff |
|
|
|
Management system and safety at work. |
|
|
|
Route map and process verification. |
|
|
|
COVID-19 Biosafety Manual, checklist and contingency measures |
|
|
|
COVID-19 Sedation Note |
|
|
|
Note for face-to-face consultation and procedures |
|
|
|
Procedure and checklist for scheduling endoscopic procedures in patients with semi-urgent and priority indications. |
|
|
|
Procedure and checklist for scheduling a face-to-face visit during a pandemic |
|
|
|
COVID-19 Sedation Procedure |
|
Table 1: Documents adapted, modified, or created for start-up in a pandemic era.
|
Pandemic COVID-19 Endoscopy Scheduling with PPE Complete Availability |
|||
|
Behavior of COVID-19 in the community |
Endoscopy service offering |
Strategy |
Average time per room |
|
Exponential increase of new cases |
None |
|
|
|
Rapid (non- exponential) increase in new cases |
_ Performing time- sensitive procedures - Postpone elective endoscopies |
- Prioritization 1, 2 and 3 |
- 1 hour |
|
Declining trend in new cases |
- Perform time- sensitive procedures -Start elective procedures |
-Priorization 1, 2 and 3 -Diagnosis in patients with risk factors - High risk screening -Cancer follow-up -Necessary to take action for other specialties |
- - 40 minutes |
|
No new cases diagnosed in the last 2 weeks |
- Normalization |
-Adding necessary diagnostic procedures without risk factors. -Follow up low grade lesions - Average risk screening |
- 30 minutos |
Table 2: Strategy for categorizing and prioritizing endoscopic procedures during a SARS-CoV-2 pandemic
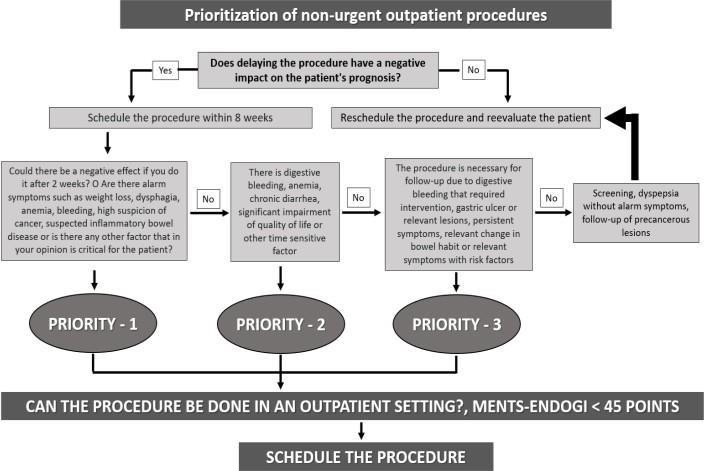
Figure 2: Flow chart for prioritization of endoscopic procedures
|
|
Figure: Scheduling of diagnostic endoscopic procedures according to covid curve
Figura 3: Ments-endogi scale
B.Programmable Endoscopic Procedure
C. Non-Programmable Endoscopic Procedure