
Tayfun Gündüz *, Muharrem Said Coşgun, Hüsnü Değirmenci, Eftal Murat Bakırcı, Halil İbrahim Tanrıseven
Erzincan Binali Yıldırım University, Faculty of Medicine, Department of Cardiology, Erzincan/Turkey
*Corresponding Author: Tayfun Gündüz, Erzincan Binali Yıldırım University Faculty of Medicine Department of Cardiology Erzincan/Turkey
Received date: April 04, 2021
Accepted date: April 10, 2021
published date: April 15, 2021
Citation: Gündüz T, Muharrem S Coşgun, Değirmenci H, Eftal M Bakırcı, Halil İ Tanrıseven. (2021) “Coronary artery to Pulmoner Artery Fistula.” J Clinical Cardiology Interventions, 2(2); DOI: http;//doi.org/04.2021/1.1015
Copyright: © 2021 Tayfun Gündüz. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Coronary artery fistulas are the second most common anomalies after coronary artery outlet anomalies. The fistula is often in the right coronary artery. It opens into the right ventricle and right atrium. It is less frequently seen in the coronary sinus, superior vena cava, pulmonary artery, and left atrium. A left-right shunt may occur as a result of the fistula. The most common symptoms are dyspnea and fatigue.
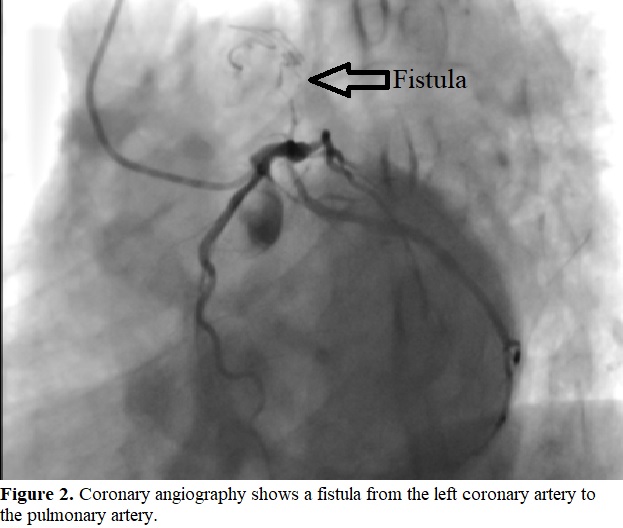
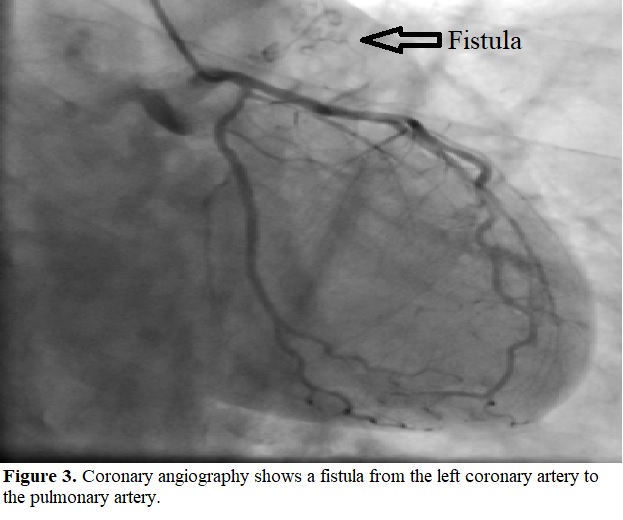
Complications such as congestive heart failure, bacterial endocarditis, myocardial infarction, and aneurysm rupture may be encountered. Coronary artery fistula is an abnormal connection between the coronary artery and the great vessels or heart cavities. Most coronary artery fistulas are diagnosed incidentally during angiography for the diagnosis of coronary artery disease. In this article, we presented a case of coronary artery to pulmonary artery fistula that we detected incidentally during coronary angiography.
Introduction
Coronary artery fistulas are the second most common coronary artery anomalies after coronary artery outflow anomalies. Congenital coronary arteriovenous fistulas (CAVF) are rare cardiac anomalies [1]. This anomaly was first described by Krause in 1865 [2]. Coronary artery fistulas are not only rare but also difficult to diagnose. Although usually congenital, acquired fistulas have also been reported. Cases acquired as complications of chest trauma, coronary angiography and bypass surgery have also been reported. Coronary artery fistulas are the connections between the coronary arteries and the chambers or veins of the heart or the pulmonary circulation that pass before the myocardiac capillary bed [3]. The fistula usually opens into the formations on the right side of the heart. The most common opening site is the right ventricle, followed by the right atrium, superior vena cava, pulmonary artery, left atrium, left ventricle and coronary sinus in order of frequency [4]. As the number of patients examined with advanced echocardiography devices and selective coronary angiography increases, the number of cases also increases. Although fistula is generally asymptomatic, It may present with symptoms and signs such as stable angina pectoris, unstable angina pectoris, myocardial infarction, and aneurysm dilatation. In this article, we presented a case of fistula from coronary artery to pulmonary artery.
Case Report
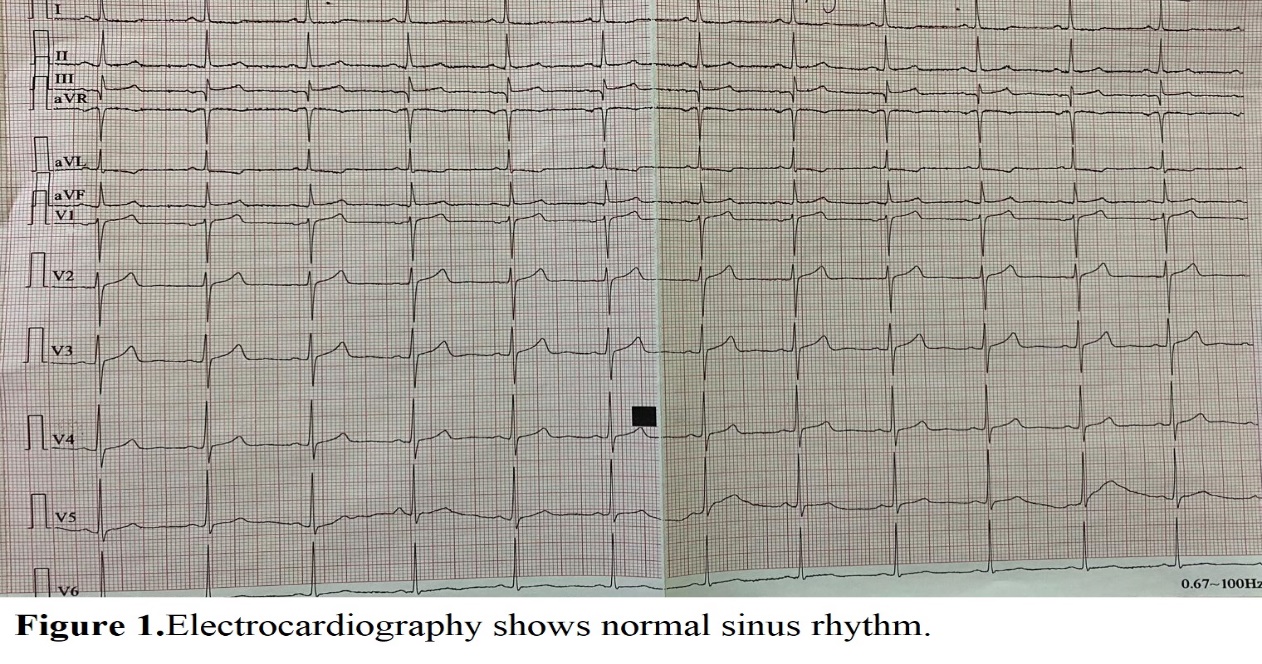
A 66-year-old patient with a previously known diagnosis of coronary artery disease and hypertension was admitted to our exertional angina clinic. The patient had a typical restless chest pain that occurred with effort for 3 weeks. Respiratory sounds and heart sounds were normal when listening to the patient. Blood pressure arteriole was 120/80 mmHg, respiratory rate was 14 / min, and pulse was 92 / min. Routine biochemical and hematological parameters were normal. Electrocardiography was in normal sinus rhythm (Figure 1). There were no additional features electrocardiographically. Transthoracic echocardiography was normal. Balloon predilection was performed, which complied with the severe lesion detected in the right coronary artery in the coronary angiography performed on the patient. In addition, a drug-coated stent was implanted. Left coronary angiography revealed a fistula from the left coronary artery to the pulmonary artery (Figure 2, Figure 3). The patient was discharged with recommendations, with antianginal and anti-event medical treatment.
Discussion
Although coronary fistula is seen with rates as low as 0.002% in the general population, it is seen between 0.05-0.25% in patients who underwent coronary angiography for any reason [5]. Coronary fistulas are mostly seen in the right coronary artery and most of them open to the right part of the heart. However, in our case, it was in the left coronary artery. Coronary fistulas often open to the right ventricle and right atrium [6]. In our case, there was a fistula from the left coronary artery to the pulmonary artery. Coronary fistulas open into veins that are particularly low pressure. They contain venous blood in the pulmonary artery and are low pressure arteries. In our case, a fistula opening into the pulmonary artery supports this information.
The clinical presentation is affected by age, the amount of left-right shunt, coronary ischemia, and the heart cavity where the fistula ends. Symptoms and signs such as fatigue, dyspnea, orthopnea, myocardial ischemia, myocardial infarction, congestive heart failure, endocarditis, arrhythmia and stroke may be observed due to shunt [7]. However, most of the adults are asymptomatic and diagnosed after examinations or tests performed for different reasons. Our patient had coronary artery disease due to atherosclerosis and a fistula from the left coronary artery to the pulmonary artery. In our patient, a stent was implanted in a severe stenosis in the right coronary artery. Our patient's clinic improved after stent was implanted in the right coronary artery. Our patient was considered asymptomatic in terms of fistula to the pulmonary artery. Fistulas should be closed in symptomatic patients, whereas in asymptomatic patients, if the risk of complications due to fistula is high, it should be closed. A continuous murmur (sometimes with trill) in the lower part of the sternum due to the fistula, effort dyspnea, tachycardia, fatigue or anginal pain are among the indications for closure. Congestive heart failure, bacterial endocarditis, myocardial infarction, and pulmonary hypertension are complications that may occur with age [8]. Our asymptomatic patient was followed up in terms of both clinical and possible complications. Pulmonary artery pressure monitoring was planned echocardiographically. In addition, he was followed up in terms of both clinical and noninvasive examinations in terms of coronary ischemia. In case of coronary ischemia in noninvasive examinations, intervention was planned if it was clinically symptomatic. Coronary fistulas can be closed by ligation of the abnormal artery, coil embolization, or open heart surgery [9].
In conclusion, percutaneous or surgical closure of coronary fistulas with symptoms and signs of coronary ischemia and a high risk of developing complications should be considered. However, fistulas that are asymptomatic or have a low risk of developing complications can be followed up with medical treatment. We should also consider that patients admitted to the clinic may have a coronary fistula.